SCHEDULE INFORMATION
PRINTABLE SCHEDULE
-
SCHEDULES
- SCHEDULE OVERVIEW
- GENERAL SESSION SCHEDULE
- PRE-COURSE SCHEDULES
- NON-PHYSICIAN TRACK SCHEDULE
- ABSTRACT SCHEDULE
-
SCHEDULE OVERVIEW
Annual Meeting Breakout Schedule
Posted:
PDF versionSUNDAY, JUNE 1 7:00 AM 4:00 PM Registration 8:00 AM 5:00 PM PRE-COURSE: Diving 8:00 AM 5:00 PM PRE-COURSE: Safety: Evaluating equipment for safe use in the hyperbaric environment 12:00 PM 1:00 PM Lunch (on own) 6:30 PM 8:30 PM Welcome Reception with AsMA MONDAY, JUNE 2 7:00 AM 4:00 PM Registration 8:00 AM 8:45 AM Opening Ceremony / Welcome Announcements / Keynote Introductions with AsMA 8:45 AM 10:00 AM Bauer Lecture with AsMA 10:00 AM 10:30 AM AsMA-UHMS Exhibits / Break 10:30 AM 11:45 AM UHMS Kindwall Keynote with AsMA: Shai Efrati, MD: The Development of Hyperbaric Medicine from Decompression to Regeneration 12:00 PM 2:00 PM Lunch (on own) Session A - HBO2 Theory and Mechanisms 2:00 PM 2:30 PM Plenary: International Panel 2:30 PM 2:40 PM oral abstract Posters: A B C 2:40 PM 2:50 PM oral abstract 2:50 PM 3:00 PM oral abstract 3:00 PM 3:30 PM Plenary: Session A 3:30 PM 4:00 PM AsMA-UHMS Exhibits / Break Session B - Clinical HBO2 4:00 PM 4:30 PM Plenary: Session B 4:30 PM 4:40 PM oral abstract Posters A B C 4:40 PM 4:50 PM oral abstract 4:50 PM 5:00 PM oral abstract 5:20 AM 5:30 PM Plenary: UHM Fellows: Top articles in Hyperbaric Medicine TUESDAY, JUNE 3 8:00 AM 4:00 PM Registration 8:30 AM 9:00 AM Announcements / Keynote Introductions with AsMA 9:00 AM 10:00 AM Reinartz Lecture with AsMA 10:00 AM 10:30 AM AsMA-UHMS Exhibits / Break 10:30 AM 11:45 AM UHMS Lambertsen Keynote with AsMA: 12:00 PM 2:00 PM Lunch (on own) Session C - Decompression Theory and Mechanisms 2:00 PM 2:30 PM Plenary: Session C 2:30 PM 2:40 PM oral abstract Posters D E F 2:40 PM 2:50 PM oral abstract 2:50 PM 3:00 PM oral abstract 3:00 PM 3:30 PM Plenary: UHMS STEM Opportunity: Virginie Papadopoulou, PhD 3:30 PM 4:00 PM AsMA-UHMS Exhibits / Break Session D - Diving Medicine 4:00 PM 4:30 PM Plenary: Session D 4:30 PM 4:40 PM oral abstract 4:40 PM 4:50 PM oral abstract 4:50 PM 5:00 PM oral abstract 5:00 PM 5:30 PM Plenary: UHM Fellows: Top articles in Undersea Medicine WEDNESDAY, JUNE 4 8:00 AM 4:00 PM Registration 8:30 AM 10:00 AM Plenary 10:00 AM 10:30 AM AsMA-UHMS Exhibits / Break Session E - HBO2 Operations, Chambers and Equipment 10:30 AM 11:00 AM Plenary: Session E 11:00 AM 11:10 AM oral abstract 11:10 AM 11:20 AM oral abstract 11:20 AM 11:30 AM oral abstract 11:30 AM 12:00 PM Plenary / orals 12:00 PM 2:00 PM Lunch (on own) Session F - Top Case Reports 2:00 PM 2:30 PM Plenary: Session F 2:30 PM 2:40 PM oral abstract 2:40 PM 2:50 PM oral abstract 2:50 PM 3:00 PM oral abstract 3:00 PM 3:30 PM Plenary / orals 3:30 PM 4:00 PM AsMA-UHMS Exhibits / Break 4:00 PM 5:30 PM RAM Bowl with AsMA 7:00 PM 10:00 PM UHMS honors night THURSDAY, JUNE 5 8:00 AM 2:00 PM Registration 7:30 AM 8:00 AM UHMS Business Meeting 8:00 AM 8:15 AM Announcements / Keynote Introductions with AsMA 8:15 AM 9:15 AM Armstrong Lecture with AsMA 9:15 AM 9:45 AM Break 9:45 AM 11:15 AM Hart Keynote (Michael Strauss, MD) 11:30 PM 1:30 PM Lunch (on own) ASSOCIATES BREAKOUT SESSION 1:30 PM 2:00 PM 2:00 PM 2:30 PM 2:30 PM 3:00 PM 3:00 PM 3:30 PM break 3:30 PM 4:00 PM 4:00 PM 4:30 PM 4:30 PM 5:00 PM 6:00 PM 9:00 PM AsMA honors night 9:00 PM 12:00 PM AsMA / UHMS after party -
GENERAL SESSION SCHEDULE
THURSDAY, JUNE 18 - SATURDAY, JUNE 20
PDF copy
Subject to change
PostedCOMING SOON
-
PRE-COURSE SCHEDULES
PRE-COURSES: WEDNESDAY, JUNE 17
FITNESS TO DIVEsubject to change: posted:
-
NON-PHYSICIAN TRACK SCHEDULE
SATURDAY, JUNE 20
Posted:
(not approved for physician CME credits)COMING SOON
-
ABSTRACT SCHEDULE
ABSTRACT SCHEDULE
POSTED: 4/10/23
FRIDAY, JUNE 16 11:30 AM 12:00 PM Posters: Session A: (A1-A2, A4) & Session B: (B5, B7-B21) -
A1: Hippocampal neuronal death partially inhibited with early hyperbaric oxygen therapy in asphyxial cardiac arrest rat model: Hyoung Youn Lee, PhD
-
A2: Oxidative burst and cytokine expression in patients and healthy volunteers receiving hyperbaric oxygen: A pilot study: Lindell K. Weaver, MD, FACP, FCCP, FCCM, FUHM
- A4: Early single-session hyperbaric oxygen therapy attenuates post cardiac arrest renal injury in asphyxial cardiac arrest rat model: YS Lee, MD
- B5: National outcomes of hyperbaric oxygen in necrotizing soft tissue infections: William Toppen, MD
- B7: Age and diabetes increase refractive changes over time with hyperbaric oxygen: Jay C. Buckey, M.D.
- B8: Pilot evaluation of long-term follow-up for the Multicenter Registry for Hyperbaric Oxygen Therapy: Jay C. Buckey, M.D.
- B9: Multicenter Hyperbaric Outcomes Registry: 2022 review: Jay C. Buckey M.D.
- B10: Retrospective assessment of the “Duke Mods”, An approach to reducing hyperbaric tender decompression sickness risk for multiplace chamber operations: M. Claire Ellis
- B11: Association between number of hyperbaric oxygen therapy sessions and neurocognitive outcomes of acute carbon monoxide poisoning: Yong Sung Cha, MD, PhD
- B12: Utility of echocardiographic global longitudinal strain to predict myocardial fibrosis in patients in carbon monoxide poisoning: Yong Sung Cha, MD, PhD
- B13: Hyperbaric oxygen therapy regimens, treated conditions, and adverse effect profile: A UHMS survey study:
Matteo Laspro, BA
- B14: Perception and availability of hyperbaric oxygen therapy as a treatment modality for carbon monoxide poisoning among emergency medicine physicians: Tyler Connely, BS
- B15: Early hyperbaric oxygen therapy is associated with favorable outcome in iatrogenic cerebral arterial gas embolism: Individual patient data meta-analysis of observational studies: Robert P. Weenink, CAPT (Navy), MD, PhD
- B16: Hyperbaric oxygen therapy chamber supervision across the usa: how often do practitioners supervise more than one HBO2 simultaneously?: Helen Gelly, MD, FUHM, UHM/ABPM
- B17: Inflammatory response profiles in COVID-19 patients treated with hyperbaric oxygen therapy compared with best practice: Anders Kjellberg, MD
- B18: The objective effects of Hyperbaric oxygen therapy on the chronic non-healing wounds using digital planimetry:
Mor Rittblat, MD
- B19: Severe digital frostbite treated with hyperbaric oxygen therapy: Jessica Hoge, MD
- B20: Effectiveness of 6-week follow-up after hyperbaric oxygen treatment for carbon monoxide poisoning in identifying delayed neurological sequelae and referral to neurological services: Dallin Lindahl, MD, MS
- B21: Oxygen concentration in and around a monoplace hyperbaric chamber after emergency decompression and defibrillation safety: Justin P. Meunier, MD
ORAL PRESENTATIONS 2:00 PM 2:10 PM B11: Association between number of hyperbaric oxygen therapy sessions and neurocognitive outcomes of acute carbon monoxide poisoning; Yong Sung Cha, MD, PhD 2:10 PM 2:20 PM B18: The objective effects of Hyperbaric oxygen therapy on the chronic non-healing wounds using digital planimetry;
Mor Rittblat, MD2:20 PM 2:30 PM A3: Sex differences in susceptibility to central nervous system oxygen toxicity: Matthew S. Makowski, MD 4:30 PM 4:40 PM B5: National outcomes of hyperbaric oxygen in necrotizing soft tissue infections: William Toppen, MD 4:40 PM 4:50 PM B6: A Randomized Trial of Preoperative Hyperbaric Oxygen (HBOT) Before Pancreaticoduodenectomy: Enrico Camporesi, MD 4:50 PM 5:00 PM B7: Age and diabetes increase refractive changes over time with hyperbaric oxygen: Jay Buckey, MD 5:00 PM 5:30 PM Posters: Session B: (B22-B41) - B22: U.S. multicenter randomized controlled trial of hyperbaric oxygen for COVID-19 patients with moderate to severe hypoxemia: Enoch Huang, MD, MPH&TM, FUHM
- B23: Hyperbaric oxygen treatment + icing achieves the effects of icing and thermotherapy simultaneously in a rat acute skeletal muscle contusion model: Takashi Hoshino MD, PhD
- B24: Dartmouth Registry Annual Report: A look at treatment of conditions outside of UHMS indications:
Hideaki Leo Tanaka, MD, FACEP
- B25: Feasibility and FDA evaluation for a Phase II Clinical Trial on efficacy of hyperbaric oxygen therapy for post COVID condition: Hideaki Leo Tanaka, MD, FACEP
- B26: Risk factors for complications of orthopedic trauma – post hoc analysis of the HOLLT Study data: Ian Millar MBBS
- B27: Assessing hyperbaric and undersea medicine physicians prescribing practices regarding HBO2 for non-emergent indications in patients who smoke: Kaighley Brett, MD
- B28: A randomized, double-blind trial of hyperbaric oxygen for persistent symptoms after brain injury (HYBOBI-2):
Lindell K. Weaver, MD, FACP, FCCP, FCCM, FUHM
- B29: Carbon monoxide poisoning from being towed behind a boat: Lindell K. Weaver, MD, FACP, FCCP, FCCM, FUHM
- B30: A 19-year retrospective analysis of hyperbaric oxygen seizures : Geness Koumandakis, RRT
- B31: Does slow and steady win the race? Consideration on optimal compression time: Samuel Hawkins, MD
- B32: CO-oximetry in the emergency department: Jeffrey Cooper, MD
- B33: Hyperbaric oxygen therapy for renal abscess: A case series: Kazuki Yanagida, MD
- B34: Current trends in hyperbaric oxygen therapy use in central retinal artery occlusion management in US hyperbaric facilities: William Toppen, MD
- B35: Neuropsychological outcomes in a randomized, double-blind trial of hyperbaric oxygen for persistent symptoms after brain injury: Rosemary Ziemnik, MS
- B36: Safety and adverse events in a randomized, double-blind trial of hyperbaric oxygen for persistent symptoms after brain injury (HYBOBI-2): Rosemary Ziemnik, MS
- B37: Hyperbaric treatment improves late effects of radiation on the chest wall: Joan Chou, MD
- B38: Successful placement and activation of artificial urethral sphincter for urinary incontinence after completing adjunctive hyperbaric oxygen therapy for radiation cystitis: Dallin Lindahl, MD, MS
- B39: Myodesopsia after hyperbaric oxygen therapy: An unusual case report: Jiho Lee, PhD
- B40: Hyperbaric oxygen therapy for thalamic pain syndrome: Peter Lennox MD
- B41: HBO2 for wound in irradiated field leads to avoidance of surgery: A case report: Jayanth Adusumalli, MBBS, MPH
SATURDAY, JUNE 17 ORAL PRESENTATIONS 10:30 AM 10:40 AM C55: Diving into decompression sickness-resistant rat’s gene expression of genes involved in antioxidant mechanisms and mitochondrial biogenesis; Emmanuel Dugrenot, PhD 10:40 AM 10:50 AM C56: Real-time deployment feasibility of deep learning VGE detection models for ultrasound echocardiograms:
Arian Azarang, PhD10:50 AM 11:00 AM C58: Effects of oxygen prebreathing on tissue nitrogen content under normobaric and hyperbaric conditions:
Edward Ashworth, PhD11:00 AM 11:10 AM C52: Elevations of inflammatory biomarkers in closed circuit SCUBA divers parallel those in DCS models: Stephen Thom, MD 11:10 AM 11:20 AM C53: A Novel Method for Observing Gaseous Nitrogen In Vivo and Ex Vivo Using Radioactive Nitrogen-13: Edward Ashworth, PhD 11:20 AM 11:30 AM C54: Preliminary qualitative assessment of bubbles inside porcine lymph nodes, imaged by ultrasound after a provocative dive profile: Josh Currens, BS 11:30 AM 12:00 PM Posters: Session B: (B42-B51) & Session C: (C54-C62) - B42: Use of hyperbaric oxygenation therapy for Cyclophosphamide-Induced Hemorrhagic Cystitis. A case report with a call for awareness and advocacy: Denise Nemeth, OMS-II, MPAS, PA-C
- B43: CT perfusion patterns in iatrogenic cerebral arterial gas embolism: a retrospective cohort study: R.A. Fakkert, MD
- B44: Hyperbaric oxygen therapy for cerebral radiation necrosis secondary to stereotactic radiation: A Case Series:
Jeffrey Cooper, MD
- B45: Incidence of COVID-19 history among patients with ISSNHL treated with hyperbaric oxygen therapy:
Jacek Kot, MD, PhD
- B46: Hyperbaric oxygen therapy for pyoderma gangrenosum as a new treatment strategy: HOTPANTS trial: Ellen C. Kop, MD, PhD
- B47: A research on the application of hyperbaric oxygen treatment for the treatment of sepsis: Xuyuan Kuang, MD, PhD
- B48: Delayed encephalopathy of tramadol overdoses related CHANTER syndrome successfully treated with consecutive hyperbaric oxygen therapy: Naoto Jingami, MD, PhD
- B49: Hyperbaric oxygen for long-covid condition: Joshua J. White, JD
- B50: Why wound you heal?: Liz Eshleman, MSN, FNP-C
- B51: E-cigarette explosion leading to oropharyngeal cancer: Jessica Coffendaffer, MSN, APRN, FNP-C
- C54: Preliminary qualitative assessment of bubbles inside porcine lymph nodes, imaged by ultrasound after a provocative dive profile: Josh Currens, BS
- C55: Diving into decompression sickness-resistant rat’s gene expression of genes involved in antioxidant mechanisms and mitochondrial biogenesis: Emmanuel Dugrenot, PhD
- C56: Real-time deployment feasibility of deep learning VGE detection models for ultrasound echocardiograms:
Arian Azarang, PhD
- C57: Automated grading of venous gas emboli in Doppler ultrasound achieves human inter-rater agreement performance: A log-scale mel spectrogram-based deep learning approach: Arian Azarang, PhD
- C58: Effects of oxygen prebreathing on tissue nitrogen content under normobaric and hyperbaric conditions:
Edward Ashworth, PhD
- C59: A PET compatible hyperbaric chamber for rodents to enable temporal and spatial monitoring of tissue nitrogen gas (nitrogen-13) in vivo: Edward Ashworth, PhD
- C60: Pathophysiology of cutis marmorata in porcine decompression sickness: Aashay Patel, BSPH
- C61: Stress and inflammation salivary analytes collected from standardized dives: Rhiannon Brenner
- C62: Measuring whole-body inert gas turnover: Oscar Plogmark, MD, PhD student
ORAL PRESENTATIONS 3:00 PM 3:10 PM D65: Preliminary evidence that fourteen days of apnea and hypoxia exposures reduces circulating pro-inflammatory microparticles: Zachary Schlader, PhD 3:10 PM 3:20 PM D66: Analysis of chest radiographs from navy SEAL (Sea Air Land) candidates developing pulmonary symptoms while swimming: Two different patterns of what previously has been described as pulmonary: Peter Lindholm, MD, PhD 3:20 PM 3:30 PM D67: Arterial PCO2 during submersed prone exercise suggests attenuation of hypercapnia after respiratory muscle training: Nicholas Bartlett 5:00 PM 5:30 PM Posters: Session C: (C63-C64) & Session D: (D68-D83) & Session F: (F117) - C63: A quantitative approach to assess similarity between dives under the Bühlmann decompression algorithm constraints: Josh Currens, BS
- C64: Analysis of gas evolution in the heart, liver and kidney of turtles presenting with decompression sickness based on ultrasonography: Katherine Eltz, BS, PhD Student
- D68: Effects of hyperbaric exposure on perceptual-motor coordination: Nozomu Kageyama , PhD
- D69: Nitrous oxide consistently attenuates thermogenic and thermoperceptual responses to repetitive cold stress in humans: Maaike Iris Moes, Msc
- D70: Relative hypoxemia at depth during breath-hold diving investigated through arterial blood gas analysis and lung ultrasound: Gerardo Bosco, MD, PhD
- D71: Evaluation and follow-up of divers after COVID-19 infection: A prospective, observational study: Charlotte Sadler, MD
- D72: Exercise-related drops in blood oxygen saturation to diagnose marginal decompression sickness cases:
Gabriela Morales, BSE
- D73: DRACO 2023: DAN looks at increased gas consumption upon return to dive in divers with COVID-19 infection:
Frauke Tillmans, PhD
- D74: Divers treated in Townsville, Australia: Worse symptoms lead to poorer outcomes: Denise F Blake, BN, MD, FRCPC, FACEM, PGDipMedSci (DHM), Dip DHM, PhD candidate
- D75: Cost effectiveness of urinalyses in occupational diver clearance: William Toppen, MD
- D76: Sampler and proposed biological test for contaminated water at dive sites: Rachel M Lance, PhD
- D77: Treatment of decompression sickness at Kawashima Orthopaedic Hospital: Masayuki Kawashima, MD
- D78: Lack of recompression facilities for diving injuries on the Central Gulf Coast: Julio R. Garcia RN, BSN, ACHRN, WCC, FAPWCA
- D79: Maximal fat oxidation in relation to 20 weeks of military diver training: Clara Sjöblom MSc
- D80: Identifying low risk dive profiles in the Canadian Diving Data and Doppler Ultrasonic Data BASE: A retrospective review: Kaighley Brett, MD
- D81: Neurocognitive performance during repetitive recreational harvesting dives: Grant Dong B.S.
- D82: From UPTD to ESOT: Monitoring hyperoxic exposure in surface-oriented diving: Jan Risberg, MD, PhD
- D83: State of the art review – Cardiac fitness assessment for diving in individuals with pre-existing asymptomatic coronary artery disease: Weien Chow, MRCP, M.Med
- F116: Bedside fluorescence microangiography aids decision-making regarding hyperbaric oxygen therapy for a compromised flap: Jenny Thacker, MD, FACEP
SUNDAY, JUNE 18 ORAL PRESENTATIONS 9:00 AM 9:30 AM E100: Rapid discharge of rechargeable lithium-ion batteries at 1ATA and 3ATA: Chae Bliss, CHT 9:30 AM 9:40 AM E92: GO/NO GO: A tool to eliminate the guesswork in determining which items may be allowed in a hyperbaric chamber:
Jeff Mize RRT, CHT, UHMSADS9:40 AM 9:50 AM E98: A solution for clinical hyperbaric facilities to easily standardize, track and document routine safety inspections: Checklist-based digital task manager: Tiffany Hamm BSN, RN, ACHRN, CWS, UHMSADS 9:50 AM 10:00 AM F123: Pneumorrhachis and pneumocephalus following epidural anesthesia for labor and delivery: A case report and systematic review: Michelle Cao, BA 2:30 PM 2:40 PM E88: A Case to Support the Routine Monitoring and Analysis of Breathing Gases Provided to the BIBS Line from Vendor Provided K Cylinder Storage: John Sullivan, CHT 2:40 PM 2:50 PM E89: Barriers to 24/7 Availability and Emergent Clinical Capabilities of Hyperbaric Medicine Facilities: A Large-Scale Survey Study: John McGlynn, MD 2:50 PM 3:00 PM E90: Strengths and Weaknesses of Monoplace vs Multiplace Chambers for Hyperbaric Critical Care: Ian Millar, MBBS 3:30 PM 4:00 PM Posters: Session D: (D84-D87) & Session E: (E88-E97; E99-E101) & Session F: (F102-F103) - D84: Redefining work of breathing: Addressing modeling gaps in instantaneous flow models: Victoria Ribeiro Rodrigues, BS, PhD Student
- D85: Determination of tidal volume-controlled buoyancy boundaries’ impact on diver workload efficiency: Aviad Cahana, BSc
- D86: Crochetage pattern: An electrocardiographic warning sign for scuba divers: Sarah Crawford MD, MSc
- D87: Development of a model to simulate underwater physiology: Tobias Cibis, PhD Candiate
- E88: A case to support the routine monitoring and analysis of breathing gases provided to the BIBS Line from vendor-provided K cylinder storage: John Sullivan, CHT
- E89: Barriers to 24/7 availability and emergent clinical capabilities of hyperbaric medicine facilities: A large-scale survey study: John J McGlynn, MD
- E90: Strengths and weaknesses of monoplace vs multiplace chambers for hyperbaric critical care: Ian Millar, MBBS
- E91: Allowing emergency decompression for inside attendant during hyperbaric oxygen therapy: Oscar Plogmark, MD, PhD student
- E93: Laptop-style POCUS machines in the multiplace HBO2 chamber: Jenny Thacker, MD, FACEP
- E94: The development of hyperbaric medicine in Korea since 2017: Sungmin Lee, MD, PhD
- E95: Evaluating the function and safety of a Bluetooth™ device in the multiplace hyperbaric environment:
Andrew Melnyczenko, BSHCA, CHT
- E96: Evaluation of an elastomeric respirator for use in the multiplace hyperbaric environment: Heather Viste, BAN, RN
- E97: Effects of airway and pressure threshold resistance on fatigue and cognition in divers: Daniel Steven Williams, BSCPE, MSEE
- E99: Predicting tidal volume of the Zoll Z Ventilator in a hyperbaric chamber: Abigail Winn, MD
- E100: Rapid discharge of rechargeable lithium-ion batteries at 1ATA and 3ATA: Chae Bliss BS, CHT, EMT
- E101: How hard is it to change from lithium-ion to alkaline fuel cell in a portable device?: Tony Turner, MAICD
ORAL PRESENTATIONS 4:00 PM 4:10 PM F102: Hyperbaric oxygen therapy in the management of upper extremity frostbite injury: A case series: Olayinka David Ajayi, MD, MPH 4:10 PM 4:20 PM F103: Fluorescence microangiography as a novel tool to identify and monitor ischemia in crush injury: Margot Samson, MD 4:20 PM 4:30 PM F104: Acute Central Retinal Artery Occlusion from Cosmetic Filler Injection: Casey Smith, MD 4:30 PM 5:00 PM Posters: Session F: (F104-F116; F118-F124) - F102: Hyperbaric oxygen therapy in the management of upper extremity frostbite injury: A case series:
Olayinka David Ajayi, MD, MPH
- F103: Fluorescence microangiography as a novel tool to identify and monitor ischemia in crush injury: Margot Samson, MD
- F104: Acute central retinal artery occlusion from cosmetic filler injection: Casey Smith, MD
- F105: New seizure disorders after carbon monoxide poisoning: Lindell K. Weaver, MD, FACP, FCCP, FCCM, FUHM
- F106: Hyperbaric oxygen treatment for paracentral acute middle maculopathy: A case study: Robert Neiberger, DO
- F107: Atypical avascular necrosis treated with hyperbaric oxygen therapy: Cheryl Hickey, MD
- F108: Acute Traumatic Polymicrobial Pinna Perichondritis Treated with Hyperbaric Oxygen Therapy:
Raymond C. Shields, MD
- F109: Hyperbaric oxygen therapy in cases of BK virus hemorrhagic cystitis: Christopher Allen, MD
- F110: Case report of an intractable cough due to radiation pneumonitis treated with hyperbaric oxygen:
Gerald H. Markovitz, MD
- F111: Polyarteritis nodosa treated with hyperbaric oxygen therapy: Jessica Hoge, MD
- F112: Hyperbaric oxygen therapy for the treatment of carbon monoxide-induced delayed neurological sequelae: A case report and review of the literature: Colin Teo, MBBS
- F113: Successful outcome from persistent brain abscess with addition of adjunctive hyperbaric oxygen therapy:
Christopher Woodard, MB, BCH, BAO
- F114: Resolution of ischemic colitis with perforation, with hyperbaric oxygen treatments: Kim Wilkinson, RN-AND
- F115: Altitude DCS treatment options: Nathan Kwan, MAJ (Army), MD
- F117: Massive venous gas embolism in a diver post-COVID: Jenny Thacker, MD, FACEP
- F118: Acute cognitive impaired diver hyperbaric treatment effect: A case series: Ian Kirby, MD, CCFP, UHM
- F119: Case report of PFO closure in an occupational diver after Type II DCS: Kaighley Brett, MD
- F120: Immersion pulmonary edema: Not limited to a specific UBA: James E. Breuer, MD
- F121: Alternate teatment For AGE when USN TT6 not feasible: Shane Day, DO, MPH, MS, CP
- F122: Good result of hyperbaric oxygen therapy in a 50 year old male with chronic therapy refractair osteomyelits on the left foot, with diabetes mellitus and sensomotoric axonal polyneuropathy: Ellen C. Kop, MD, PhD
- F123: Pneumorrhachis and pneumocephalus following epidural anesthesia for labor and delivery: A case report and systematic review: Michelle Cao, BA
- F124: Unusual Presentation of Diplopia and Oxygen Toxicity Symptoms after 100% Oxygen Closed Circuit Rebreather Diving: A Case Report: Chiew Wenqi, MBBS
-
-
Keynote Lectures
- Christian J. Lambertsen Memorial Lecture
- Eric P. Kindwall Memorial Lecture
- Jefferson C. Davis Keynote
-
CHRISTIAN J. LAMBERTSEN, MD, DSc (Hon) MEMORIAL KEYNOTE
GUEST SPEAKER:
LECTURE TITLE:
Wednesday, June 4: 8:30 am - 10 am
About the Lecture:
About the Speaker:
CHRISTIAN J. LAMBERTSEN, MD, DSc (Hon) MEMORIAL KEYNOTE LECTURE
About Dr. Lambertsen:
Dr. Christian J. Lambertsen received a B.S. Degree from Rutgers University in 1938 and a M.D. Degree from the University of Pennsylvania in 1943. During his medical school period, he invented and first used forms of the initial U.S. self-contained closed-circuit oxygen rebreathing apparatus, for neutral buoyancy underwater swimming and diving. As a student, he aided the early Office of Strategic Services (O.S.S.) in establishing the first cadres of U.S. military operational combat swimmers. Dr. Lambertsen became a U.S. Army medical officer on graduation from medical school in early 1943, and immediately joined the O.S.S. Maritime Unit on active duty through its period of function in World War II. He joined the University of Pennsylvania Medical Faculty in 1946, and became Professor of Pharmacology in 1952. While a faculty member he combined diving research and further underwater rebreathing equipment developments for the Army and Navy. In 1967 he served as Founding President of the Undersea Medical Society (now Undersea and Hyperbaric Medical Society.) Dr. Lambertsen is recognized by the Naval Special Warfare community as "The Father of U.S. Combat Swimming.” His hand has touched every aspect of military and commercial diving. Dr. Lambertsen’s active contributions to diving began during WWII and became even more progressive in the post-war period through the evolutions of the U.S. Navy Deep Submergence and Naval Special Warfare developmental programs.
-
ERIC P. KINDWALL, MD MEMORIAL KEYNOTE
GUEST SPEAKER:
LECTURE TITLE:
Monday, June 2: 10:30 am - 12 pm
About the Lecture:
About the Speaker:
ERIC P. KINDWALL, MD MEMORIAL KEYNOTE LECTURE
About Dr. Kindwall: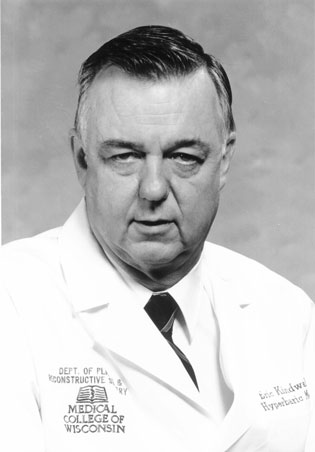 Dr. Kindwall is known by so many as the "Father of Hyperbaric Medicine.” Whether you knew him personally or simply by reputation, we have all benefited from his efforts, passion, wisdom, knowledge, energy and vision. Dr. Kindwall has played a great role in growing and shaping the specialty of Undersea and Hyperbaric Medicine. He was likewise instrumental in molding the UHMS into what it is today. Dr. Kindwall began diving in 1950. He cultivated his interest in the field and during the Vietnam War served as the Assistant Director of the U.S. Navy School of Submarine Medicine. He also was the Senior Officer responsible for the Diving Medicine Program. In 1969, after leaving the Navy, Dr. Kindwall became Chief of the Department of Hyperbaric Medicine at St. Luke’s Medical Center, Milwaukee, Wis. Shortly after the Undersea Medical Society was created in the mid-1960s, Dr. Kindwall identified the need for standardized education in the field. He created the UMS Education and Standards Committee to help elevate course content and ensure instructor competence. This committee later became our Education Committee. When the AMA initiated its Continuing Medical Education program, Dr. Kindwall persuaded the organization to recognize the UMS as a grantor of CME credits. In 1972, Dr. Kindwall felt that the Society’s members would benefit from improved communication. He created our first newsletter and was named editor. Dr. Kindwall chose the name Pressure because clinical hyperbaric medicine was rapidly developing. Even though the UHMS had not yet incorporated "Hyperbaric” into the Society’s name, he wanted a title for the newsletter that would encompass all who worked with increased atmospheric pressure. He stated: "The Society’s goal then, as it is now, is to serve all who deal with the effects of increased barometric pressure.” That same year, Dr. Kindwall recognized the need to have a relationship with Medicare to help provide insight on reputable clinical management. The UMS followed this lead, and a Medicare Panel was created. The recommendations were presented to the U.S. Public Health Service. The challenge was that no reliable hyperbaric medicine clinical guidelines were available that addressed appropriate applications of Hyperbaric Medicine. To remedy this deficit, the UMS Executive Committee created an Ad Hoc Committee on hyperbaric oxygen therapy. Dr. Kindwall was named Chair. The committee created the first Hyperbaric Oxygen Therapy Committee Report. Again, this text was published 10 years before the UHMS incorporated "Hyperbaric” into its name. The report was sent to HCFA and the Blues and became their source document for reimbursement. Dr. Kindwall updated the text two more times and thus was the Editor and Chair of the Committee and text for three of its 12 editions. Dr. Kindwall later worked to expand the available information on the specialty by creating one of the first complete texts on the field. He created Hyperbaric Medicine Practice in 1994 and later updated and revised his text two more times. The Society’s first journal, Hyperbaric Oxygen Review, has also has been influenced by Dr. Kindwall. His love for research and education was clear: He became the initial editor, creating a journal that at first consisted of review articles and one original contribution. Over the years,it has grown to one full of original research. Dr. Kindwall’s presence is felt in so many of the UHMS’ activities and initiatives. Much of what we all take for granted – what is just "there” and "available” – has his touch and influence. Some of us have been blessed to have had a closer impact by Dr. Kindwall’s life, but I think that I can easily say that each of us has been influenced in some way.
Dr. Kindwall is known by so many as the "Father of Hyperbaric Medicine.” Whether you knew him personally or simply by reputation, we have all benefited from his efforts, passion, wisdom, knowledge, energy and vision. Dr. Kindwall has played a great role in growing and shaping the specialty of Undersea and Hyperbaric Medicine. He was likewise instrumental in molding the UHMS into what it is today. Dr. Kindwall began diving in 1950. He cultivated his interest in the field and during the Vietnam War served as the Assistant Director of the U.S. Navy School of Submarine Medicine. He also was the Senior Officer responsible for the Diving Medicine Program. In 1969, after leaving the Navy, Dr. Kindwall became Chief of the Department of Hyperbaric Medicine at St. Luke’s Medical Center, Milwaukee, Wis. Shortly after the Undersea Medical Society was created in the mid-1960s, Dr. Kindwall identified the need for standardized education in the field. He created the UMS Education and Standards Committee to help elevate course content and ensure instructor competence. This committee later became our Education Committee. When the AMA initiated its Continuing Medical Education program, Dr. Kindwall persuaded the organization to recognize the UMS as a grantor of CME credits. In 1972, Dr. Kindwall felt that the Society’s members would benefit from improved communication. He created our first newsletter and was named editor. Dr. Kindwall chose the name Pressure because clinical hyperbaric medicine was rapidly developing. Even though the UHMS had not yet incorporated "Hyperbaric” into the Society’s name, he wanted a title for the newsletter that would encompass all who worked with increased atmospheric pressure. He stated: "The Society’s goal then, as it is now, is to serve all who deal with the effects of increased barometric pressure.” That same year, Dr. Kindwall recognized the need to have a relationship with Medicare to help provide insight on reputable clinical management. The UMS followed this lead, and a Medicare Panel was created. The recommendations were presented to the U.S. Public Health Service. The challenge was that no reliable hyperbaric medicine clinical guidelines were available that addressed appropriate applications of Hyperbaric Medicine. To remedy this deficit, the UMS Executive Committee created an Ad Hoc Committee on hyperbaric oxygen therapy. Dr. Kindwall was named Chair. The committee created the first Hyperbaric Oxygen Therapy Committee Report. Again, this text was published 10 years before the UHMS incorporated "Hyperbaric” into its name. The report was sent to HCFA and the Blues and became their source document for reimbursement. Dr. Kindwall updated the text two more times and thus was the Editor and Chair of the Committee and text for three of its 12 editions. Dr. Kindwall later worked to expand the available information on the specialty by creating one of the first complete texts on the field. He created Hyperbaric Medicine Practice in 1994 and later updated and revised his text two more times. The Society’s first journal, Hyperbaric Oxygen Review, has also has been influenced by Dr. Kindwall. His love for research and education was clear: He became the initial editor, creating a journal that at first consisted of review articles and one original contribution. Over the years,it has grown to one full of original research. Dr. Kindwall’s presence is felt in so many of the UHMS’ activities and initiatives. Much of what we all take for granted – what is just "there” and "available” – has his touch and influence. Some of us have been blessed to have had a closer impact by Dr. Kindwall’s life, but I think that I can easily say that each of us has been influenced in some way. -
Jefferson C. Davis Memorial Keynote
GUEST SPEAKER:
LECTURE TITLE:
Thursday, June 5: 10 am - 11 am
About the Lecture:
About the Speaker:
JEFFERSON C. DAVIS, MD KEYNOTE LECTURE
About Dr. Davis: Dr. Jefferson C. Davis devoted his entire adult life serving the diving, aerospace and hyperbaric communities. Through his clinical practice, educational activities, and publications, he inspired several generations of clinicians to provide quality medical service for divers, aviators, and hyperbaric medicine & wound care patients.
Dr. Jefferson C. Davis devoted his entire adult life serving the diving, aerospace and hyperbaric communities. Through his clinical practice, educational activities, and publications, he inspired several generations of clinicians to provide quality medical service for divers, aviators, and hyperbaric medicine & wound care patients. Dr. Davis was born December 7, 1932, and raised in Neosho, Missouri. After receiving his MD at the University of Missouri in 1958, he joined the US Air Force Medical Corps to become a flight surgeon. He received his MPH from the University of California at Berkeley and was board certified in Aerospace Medicine. He studied diving medicine at the US Navy Experimental Diving Unit in Washington DC. In 1965, Dr. Davis and his colleagues created the first US Air Force course in Hyperbaric Medicine. He founded “LEOFAST,” the US Air Force predecessor of Divers Alert Network. In 1974 he founded and became the first Director of the USAF Hyperbaric Medicine Center at Brooks Air Force Base Texas, which now bears his name. He created the Davis Protocol in the application of Hyperbaric Medicine for wound healing enhancement. He became Medical Director for Medical Seminars’ Medicine of Diving Program in which physicians from all medical specialties could learn to treat injured divers and to serve as consults to their local diving communities. In 1979, after 20 years of service Dr. Davis retired from the US Air Force as a Chief Flight Surgeon in the grade of Colonel. Dr. Davis became founding member and president of International ATMO, Inc. the first know contract provider of wound care and hyperbaric medicine services. He set up a successful practice at two San Antonio hospitals.
His compassion for his patient’s well-being was legendary and he contributed much to the diving, aerospace and hyperbaric medicine communities.
-
Continuing Education Credits: Annual Meeting
Continuing Education Credits
-In order to receive continuing education credits you must complete and submit an evaluation-
Accreditation Statement:
The Undersea and Hyperbaric Medical Society is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.Designation Statements:
- Physician CME: The Undersea and Hyperbaric Medical Society designates this live activity for a maximum of TBD AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
- Nursing/RRT Contact Hours: This live activity is approved for TBD CE hours provided by Florida Board of Registered Nursing/RRT Provider #50-10881. License types: RN, LPN, CNS, ARNP, CNA, CRT, RRT, RCP Provided through the Florida State Board of Nursing and the CE credits are reciprocal and approved for nurses within all states. Receiving credit for Florida providers is simple, attend the course and our staff will upload your credits directly to the Florida State database. For out of state credit, we provide this letter for you to file with the respective nursing board.
- NBDHMT: This live activity is approved for TBD* Category A credit hours by National Board of Diving and Hyperbaric Medical Technology, P.O. Box 758, Pelion, South Carolina 29123. *Up to TBD Cat A credits for the in-person/live stream meeting and up to TBD Cat A credits for reviewing poster review/quiz online at your leisure. Not to exceed 20 total maximum Cat A credit hours. CLICK HERE for approved lectures & posters.
- NBDHMT Accreditation Statement: For CHT recertification purposes, the NBDHMT requires a minimum of nine of the minimum 12 required Category A credits relate directly to any combination of hyperbaric operations, related technical aspects and chamber safety.
Full Disclosure Statement: Individuals in control of content participating in continuing medical education activities sponsored by Undersea and Hyperbaric Medical Society are expected to disclose to the participants any relevant financial relationships with ineligible companies. Full disclosure of faculty and planner relevant financial relationships will be made at the activity.
Disclosure:The following individuals have disclosed a relevant financial relationship with ineligible companies. Financial relationships are relevant if the following three conditions are met for the individual who will control content of the education:
A financial relationship, in any amount, exists between the person in control of content and an ineligible company and;
- The content of the education is related to the products of an ineligible company with whom the person has a financial relationship and;
- The financial relationship existed during the past 24 months.
- All of the relevant financial relationships listed for these individuals have been mitigated.
- None of the individuals in control of content (planners/faculty/reviewers/authors) for this educational activity have relevant financial relationship(s) to disclose with ineligible companies whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
- The following commercial support was received for this activity.
- Fink Engineering, unrestricted educational grant $6500
- Hyperbaric Modular Systems, Inc,. financial support: $2500
Disclaimer: The information provided at this CME activity is for Continuing Medical Education purposes only. The lecture content, statements or opinions expressed however, do not necessarily represent those of the Undersea and Hyperbaric Medical Society.Note for ABMS Board Certified Physicians: Some ABMS boards will accept accredited CME towards their MOC requirements. As an accredited provider, the UHMS can now register educational activities as CME for MOC (Part II) for ACCME collaborating boards. Please review the learner instructions and submit the necessary requirements for your credit to be reported within 30 days of course closing. Learner CME credit must be reported no later than December 1st of the reporting year. If your board is not collaborating yet with ACCME to report CME for MOC, please continue to submit your credits to your certifying board directly.
Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to:
- 20MOC points in the American Board of Anesthesiology (ABA) Maintenance of Certification(MOC) program; and
- 20MOC points in the American Board of Internal Medicine's (ABIM) Maintenance ofCertification (MOC) program; and
- 20MOC points in the American Board of American Board of Otolaryngology – Head and Neck Surgery (ABOHNS) Continuing Certification Program (CCP); and
- 20MOC points in the American Board of Orthopaedic Surgery (ABOS) Maintenance of Certification (MOC) program; and
- 20MOC points in the American Board of Pathology (ABPath) Continuing Certification Program (CCP); and
- 20MOC points in the American Board of Surgery (ABS) Maintenance of Certification (MOC) program; and
- 20MOC points in the American Board of Pediatrics’ (ABP) Maintenance of Certification(MOC) program; and
- 20MOC points in the American Board of Thoracic Surgery (ABTS) Maintenance of Certification(MOC) program.
CME For MOC Program Guide Designation Statements for ABMS Boards
Required instructions to learners on how to obtain CME for MOC
CME For MOC points are earned through completing a comprehensive evaluation component that assesses individual learner competence, performance, and/or the impact on patient outcomes. Some boards require evaluation feedback that will include a summary of what was discussed and the best next steps for the learner. The evaluation feedback will be provided to you upon submitting the evaluation form.
As an accredited ACCME provider, the UHMS is now responsible to submit physician learner CME credits into the ACCME PARS system. However, it is the physician’s responsibility to submit the necessary information required to match with the ACCME PARS system. It is also the physicians responsibility to check with their respective board(s) to see that the credits were applied accordingly.
- American Board of Anesthesiology (ABA)
“This activity contributes to the CME component of the American Board of Anesthesiology’s redesigned Maintenance of Certification in AnesthesiologyTM (MOCA®) program, known as MOCA 2.0®. Please consult the ABA website, www.theABA.org, for a list of all MOCA 2.0 requirements.” - American Board of Internal Medicine (ABIM)***
“Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn up to [credits approved] MOC points in the American Board of Internal Medicine’s (ABIM) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit participant completion information to ACCME for the purpose of granting ABIM MOC credit.” - American Board of Otolaryngology – Head and Neck Surgery (ABOHNS) ***
“Successful completion of this CME activity, which includes participation in the evaluation component, enables the participant to earn their required annual part II self-assessment credit in the American Board of Otolaryngology – Head and Neck Surgery’s Continuing Certification program (formerly known as MOC). It is the CME activity provider's responsibility to submit participant completion information to ACCME for the purpose of recognizing participation.” - American Board of Orthopaedic Surgery (ABOS) ***
“Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn credit toward the CME of the American Board of Orthopaedic Surgery’s Maintenance of Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABOS credit." - American Board of Pathology (ABPath)
This activity has been registered to offer [credits approved] AMA PRA Category 1 CreditsTM towards the American Board of Pathology’s Continuing Certification program Lifelong Learning credits. - American Board of Pediatrics (ABP) ***
“Successful completion of this CME activity, which includes participation in the evaluation component, enables the learner to earn up to [credits approved] MOC points in the American Board of Pediatrics’ (ABP) Maintenance of Certification (MOC) program. It is the CME activity provider’s responsibility to submit learner completion information to ACCME for the purpose of granting ABP MOC credit.” - American Board of Surgery (ABS) ***
“Successful completion of this CME activity [which includes participation in the evaluation component], enables the learner to earn credit toward the CME [and Self-Assessment] requirement(s) of the American Board of Surgery’s Continuous Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABS credit." - American Board of Thoracic Surgery (ABTS) ***
“Successful completion of this CME activity [which includes participation in the evaluation component,] enables the learner to earn credit toward the CME [and Self-Assessment] of the American Board of Thoracic Surgery’s Maintenance of Certification program. It is the CME activity provider's responsibility to submit learner completion information to ACCME for the purpose of granting ABTS credit."
***Will require evaluation feedback -
Social Events
Sunday, June 1
- New Members / New Attendees Meet n' Greet:
- Time: 6 pm - 6:30 pm
- Location: TBA
- Welcome Reception with Exhibitor
- Time: 6:30 pm - 8:30 pm
- Location: Grand Hall West
Monday, June 2
- Richard B Trumbo 5K Fun Run/Walk
- Time: 6:30 am - 8 am
- Location: TBA
Tuesday, June 3
- Joint Social (advance purchase): hosted by Life Sciences & Biomedical Engineering Branch (LSBEB)
- Time: 7:30 pm - 10:30 pm
- Location: TBA
Wednesday, June 4
- UHMS Honors Night (advance purchase required) aka UHMS Awards Banquet
- Time: 7 pm - 10 pm
- Location: TBA
Thursday, June 5
- AsMA Honors Night (advance purchase required)
- Time: 6 pm - 9 pm
- Location: TBA
- ASMA-UHMS After Party
- Time: 9 pm - 12 mid-night
- Location: TBA
MORE TO COME - New Members / New Attendees Meet n' Greet:
-
Committee Meeting Schedule
Committee Meetings/Luncheons Schedule
SUBJECT TO CHANGE
posted 6/5/24
Please contact lisa@uhms.org to schedule.
<BACK>
TIME DAY COMMITTEE/LUNCHEON ROOM 1700-1800 Wednesday, June 12 UHMS Diving Committee pre-course room 0700-0800 Thursday, June 13 GME Committee Burgundy 1200-1300 Thursday, June 13 FDA Liaison Committee St. Louis 1200-1300 Thursday, June 13 Education Committee Burgundy 1200-1400 Thursday, June 13 HBO2 Therapy Committee Iberville 1300-1400 Thursday, June 13 CAE Steering Committee St. Louis 1300-1400 Thursday, June 13 Research Committee Bienville 0700-0800 Friday, June 14 Presidents Breakfast (UHMS BOD Current & Past Presidents Only – Ticket required for meal) St. Ann 1200-1300 Friday, June 14 Safety Committee Burgundy 1200-1300 Friday, June 14 BNA Luncheon: 12pm-1pm (advance purchase only) Bienville 1200-1300 Friday, June 14 Publications Committee Iberville 1200-1300 Friday, June 14 STEM Committee Bienville 1300-1400 Friday, June 14 UHMJ Editorial Board St. Louis 1300-1400 Friday, June 14 QUARC Committee Burgundy 1300-1400 Friday, June 14 BNA Board meeting Bienville 0700-0800 Saturday, June 15 ACEP Committee Meeting St. Ann 1300-1400 Saturday, June 15 UHMS Associate Luncheon: 1pm-2pm (advance purchase only) St. Charles B 1300-1400 Saturday, June 15 Multicenter Registry for Hyperbaric Oxygen Treatment Steering Committee Iberville 1300-1400 Saturday, June 15 UHMS Accreditation Council Bienville 1300-1400 Saturday, June 15 Inside Attendant Committee Royal Board Room -
NBDHMT ASM23 Approved Category A Credits
Category A Credits: ASM 23
- NBDHMT:This live activity is approved for a maximum of 20* Category A credit hours by National Board of Diving and Hyperbaric Medical Technology, P.O. Box 758, Pelion, South Carolina 29123. *Up to 15 Cat A credits for the in-person/live stream meeting and up to 5 Cat A credits for reviewing posters/quiz online at your leisure. Not to exceed 20 total maximum Cat A credit hours.
- NBDHMT Accreditation Statement: For CHT recertification purposes, the NBDHMT requires a minimum of nine of the minimum 12 required Category A credits relate directly to any combination of hyperbaric operations, related technical aspects and chamber safety.
In-Person / Live Stream Credits (evaluation must be completed): up to 15 Cat A Credit hours.
Credits FRIDAY, JUNE 16 0.5 8:00 AM 8:30 AM Opening Ceremony / Welcome - UHMS President: Pete Witucki, MD 1 10:00 AM 11:30 AM Plenary: International Panel: Oxygen: How much, How Often: Jacek Kot, MD; Gerardo Bosco, MD; Tino Balestra, MSc, PhD 0.5 11:30 AM 12:00 PM Posters: Session A: (A1-A2, A4) & Session B: (B5, B7-B21) 0.2 2:20 PM 2:30 PM A3: Sex differences in susceptibility to central nervous system oxygen toxicity: Matthew S. Makowski, MD 0.5 2:30 PM 3:00 PM Plenary: UHM Fellows: Top Articles in Hyperbaric Medicine: Claire Ellis, MD: Duke Fellow 0.5 5:00 PM 5:30 PM Posters: Session B: (B22-B41) SATURDAY, JUNE 17 1 9:30 AM 10:30 AM Plenary: Session C: Decompression Panel: Stephen Thom, MD (Microparticles); David Doolette, MD (VGE Measurement); Greg Murphy (USN Heliox Tables) 0.2 10:30 AM 10:40 AM C55: Diving into decompression sickness-resistant rat’s gene expression of genes involved in antioxidant mechanisms and mitochondrial biogenesis; Emmanuel Dugrenot, PhD 0.17 10:40 AM 10:50 AM C56: Real-time deployment feasibility of deep learning VGE detection models for ultrasound echocardiograms; Arian Azarang, PhD 0.17 10:50 AM 11:00 AM C58: Effects of oxygen prebreathing on tissue nitrogen content under normobaric and hyperbaric conditions; Edward Ashworth, PhD 0.17 11:00 AM 11:10 AM C52: Elevations of inflammatory biomarkers in closed circuit SCUBA divers parallel those in DCS models: Stephen Thom, MD 0.19 11:10 AM 11:20 AM C53: A Novel Method for Observing Gaseous Nitrogen In Vivo and Ex Vivo Using Radioactive Nitrogen-13: Edward Ashworth, PhD 0.2 11:20 AM 11:30 AM C54: Preliminary qualitative assessment of bubbles inside porcine lymph nodes, imaged by ultrasound after a provocative dive profile: Josh Currens, BS 0.5 11:30 AM 12:00 PM Posters: Session B: (B42-B51) & Session C: (C54-C62) 1 2:00 PM 3:00 PM Plenary: Session D: Diving Medicine Research Panel: Richard Moon, MD; Jay Dean, MD; Jim Chimiak, MD 0.2 3:00 PM 3:10 PM D65: Preliminary evidence that fourteen days of apnea and hypoxia exposures reduces circulating pro-inflammatory microparticles: Zachary Schlader, PhD 3:20 PM 3:30 PM D67: Arterial PCO2 during submersed prone exercise suggests attenuation of hypercapnia after respiratory muscle training: Nicholas Bartlett 0.5 4:00 PM 4:30 PM Plenary: UHM Fellows: Top articles in Undersea Medicine: Matthew Makowski, MD - Duke Fellow 0.5 4:30 PM 5:00 PM Plenary: ADCI Medical Guidelines Update: Tony Alleman, MD 0.5 5:00 PM 5:30 PM Posters: Session C: (C63-C64) & Session D: (D68-D83) & Session F: (F117) SUNDAY, JUNE 18 1 8:00 AM 9:00 AM Davis Keynote: Historical perspective: Safety development; John Feldmeier, DO 0.5 9:00 AM 9:30 AM E100: Rapid discharge of rechargeable lithium-ion batteries at 1ATA and 3ATA: Chae Bliss, CHT 0.2 9:30 AM 9:40 AM E92: GO/NO GO: A tool to eliminate the guesswork in determining which items may be allowed in a hyperbaric chamber: Jeff Mize RRT, CHT, UHMSADS 0.2 9:40 AM 9:50 AM E98: A solution for clinical hyperbaric facilities to easily standardize, track and document routine safety inspections: Checklist-based digital task manager: Tiffany Hamm BSN, RN, ACHRN, CWS, UHMSADS 9:50 AM 10:00 AM F123: Pneumorrhachis and pneumocephalus following epidural anesthesia for labor and delivery: A case report and systematic review: Michelle Cao, BA 0.5 10:30 AM 11:00 AM Plenary: Review of Emergency Decompression - bailouts: Sean Hardy, MD 2 11:00 AM 1:00 PM Plenary: Risk & Liability in the hyperbaric department (technician, nurse, physician) Panel 0.5 2:00 PM 2:30 PM Plenary: Session E: Pitfalls in hyperbaric facility safety management: Francois Burman, PR ENG, BSC (ENG), MSC 0.2 2:30 PM 2:40 PM E88: A Case to Support the Routine Monitoring and Analysis of Breathing Gases Provided to the BIBS Line from Vendor Provided K Cylinder Storage: John Sullivan, CHT 0.2 2:40 PM 2:50 PM E89: Barriers to 24/7 Availability and Emergent Clinical Capabilities of Hyperbaric Medicine Facilities: A Large-Scale Survey Study: John McGlynn, MD 0.2 2:50 PM 3:00 PM E90: Strengths and Weaknesses of Monoplace vs Multiplace Chambers for Hyperbaric Critical Care: Ian Millar, MBBS 0.5 3:30 PM 4:00 PM Posters: Session D: (D84-D87) & Session E: (E88-E97; E99-E101) & Session F: (F102-F103) 0.5 4:30 PM 5:00 PM Posters: Session F: (F104-F116; F118-F124) 15 Total Cat. A credits Up to 5 Cat A credits for reviewing approved posters and submitting a quiz online at your leisure. Below is the list of the approved posters. Links will be provided after attendance.
- Friday, June 16: 11:30 am - 12:00 pm
B 10: Retrospective assessment of the “Duke Mods”, An approach to reducing hyperbaric tender decompression sickness risk for multiplace chamber operations
Presenting Author: M. Claire Ellis - Friday, June 16: 11:30 am - 12:00 pm
B 13: Hyperbaric oxygen therapy regimens, treated conditions, and adverse effect profile: A UHMS survey study
Presenting Author: Matteo Laspro, BA - Friday, June 16: 11:30 am - 12:00 pm
B 15: Early hyperbaric oxygen therapy is associated with favorable outcome in iatrogenic cerebral arterial gas embolism: Individual patient data meta-analysis of observational studies
Presenting Author: Robert P. Weenink, CAPT (Navy), MD, PhD - Friday, June 16: 11:30 am - 12:00 pm
B 21: Oxygen concentration in and around a monoplace hyperbaric chamber after emergency decompression and defibrillation safety
Presenting Author: Justin P. Meunier, MD - Friday, June 16: 5:00 pm - 5:30 pm
B 27: Assessing hyperbaric and undersea medicine physicians prescribing practices regarding HBO2 for non-emergent indications in patients who smoke
Presenting Author: Kaighley Brett, MD - Friday, June 16: 5:00 pm - 5:30 pm
B 30: A 19-year retrospective analysis of hyperbaric oxygen seizures
Presenting Author: Geness Koumandakis, RRT - Friday, June 16: 5:00 pm - 5:30 pm
B 31: Does slow and steady win the race? Consideration on optimal compression time
Presenting Author: Samuel Hawkins, MD - Friday, June 16: 5:00 pm - 5:30 pm
B 36: Safety and adverse events in a randomized, double-blind trial of hyperbaric oxygen for persistent symptoms after brain injury (HYBOBI-2)
Presenting Author: Rosemary Ziemnik, MS - Saturday, June 17: 5:00 pm - 5:30 pm
B 39: Myodesopsia after hyperbaric oxygen therapy: An unusual case report
Presenting Author: Sangwon Ko, MD - Saturday, June 17: 11:30 am - 12:00 pm
B 43: CT perfusion patterns in iatrogenic cerebral arterial gas embolism: a retrospective cohort study
Presenting Author: R.A. Fakkert, MD - Saturday, June 17: 11:30 am - 12:00 pm
C 57: Automated grading of venous gas emboli in Doppler ultrasound achieves human inter-rater agreement performance: A log-scale mel spectrogram-based deep learning approach
Presenting Author: Arian Azarang, PhD - Saturday, June 17: 11:30 am - 12:00 pm
C 59: A PET compatible hyperbaric chamber for rodents to enable temporal and spatial monitoring of tissue nitrogen gas (nitrogen-13) in vivo
Presenting Author: Edward Ashworth, PhD - Saturday, June 17: 11:30 am - 12:00 pm
C 60: Pathophysiology of cutis marmorata in porcine decompression sickness
Presenting Author: Aashay Patel, BSPH - Saturday, June 17: 11:30 am - 12:00 pm
C 61: Stress and inflammation salivary analytes collected from standardized dives
Presenting Author: Rhiannon Brenner - Saturday, June 17: 11:30 am - 12:00 pm
C 62: Measuring whole-body inert gas turnover
Presenting Author: Oscar Plogmark, MD, PhD student - Saturday, June 17: 5:00 pm - 5:30 pm
C 63: A quantitative approach to assess similarity between dives under the Bühlmann decompression algorithm constraints
Presenting Author: Josh Currens, BS - Saturday, June 17: 5:00 pm - 5:30 pm
D 72: Exercise-related drops in blood oxygen saturation to diagnose marginal decompression sickness cases
Presenting Author: Gabriela Morales, BSE - Saturday, June 17: 5:00 pm - 5:30 pm
D 74: Divers treated in Townsville, Australia: Worse symptoms lead to poorer outcomes
Presenting Author: Dr Denise F Blake, BN, MD, FRCPC, FACEM, PGDipMedSci (DHM), Dip DHM, PhD candidate - Saturday, June 17: 5:00 pm - 5:30 pm
D 77: Treatment of decompression sickness at Kawashima Orthopaedic Hospital
Presenting Author: Masayuki Kawashima, MD - Saturday, June 17: 5:00 pm - 5:30 pm
D 78: Lack of recompression facilities for diving injuries on the Central Gulf Coast
Presenting Author: Julio R. Garcia RN, BSN, ACHRN, WCC, FAPWCA - Saturday, June 17: 5:00 pm - 5:30 pm
D 82: From UPTD to ESOT: Monitoring hyperoxic exposure in surface-oriented diving
Presenting Author: Jan Risberg, MD, PhD - Saturday, June 17: 5:00 pm - 5:30 pm
D 83: State of the art review – Cardiac fitness assessment for diving in individuals with pre-existing asymptomatic coronary artery disease
Presenting Author: Weien Chow, MRCP, M.Med - Sunday, June 18: 3:00 pm - 3:30 pm
E 88: A case to support the routine monitoring and analysis of breathing gases provided to the BIBS Line from vendor-provided K cylinder storage
Presenting Author: John Sullivan, CHT - Sunday, June 18: 3:00 pm - 3:30 pm
E 89: Barriers to 24/7 availability and emergent clinical capabilities of hyperbaric medicine facilities: A large-scale survey study
Presenting Author: John J McGlynn, MD - Sunday, June 18: 3:00 pm - 3:30 pm
E 90: Strengths and weaknesses of monoplace vs multiplace chambers for hyperbaric critical care
Presenting Author: Ian Millar, MBBS - Sunday, June 18: 3:00 pm - 3:30 pm
E 91: Allowing emergency decompression for inside attendant during hyperbaric oxygen therapy
Presenting Author: Oscar Plogmark, MD, PhD student - Sunday, June 18: 3:00 pm - 3:30 pm
E 93: Laptop-style POCUS machines in the multiplace HBO2 chamber
Presenting Author: Jenny Thacker, MD, FACEP - Sunday, June 18: 3:00 pm - 3:30 pm
E 95: Evaluating the function and safety of a Bluetooth™ device in the multiplace hyperbaric environment
Presenting Author: Andrew Melnyczenko, BSHCA, CHT - Sunday, June 18: 3:00 pm - 3:30 pm
E 96: Evaluation of an elastomeric respirator for use in the multiplace hyperbaric environment
Presenting Author: Heather Viste, BAN, RN - Sunday, June 18: 3:00 pm - 3:30 pm
E 99: Predicting tidal volume of the Zoll Z Ventilator in a hyperbaric chamber
Presenting Author: Abigail Winn, MD - Sunday, June 18: 3:00 pm - 3:30 pm
E 101: How hard is it to change from lithium-ion to alkaline fuel cell in a portable device?
Presenting Author: Tony Turner, MAICD - Sunday, June 18: 4:30 pm - 5:00 pm
F 115: Altitude DCS treatment options
Presenting Author: Nathan Kwan, MAJ (Army), MD - Sunday, June 18: 4:30 pm - 5:00 pm
F 118: Acute cognitive impaired diver hyperbaric treatment effect: A case series
Presenting Author: Ian Kirby, MD, CCFP, UHM - Sunday, June 18: 4:30 pm - 5:00 pm
F 119: Case report of PFO closure in an occupational diver after Type II DCS
Presenting Author: Kaighley Brett, MD - Sunday, June 18: 4:30 pm - 5:00 pm
F 121: Alternate teatment For AGE when USN TT6 not feasible
Presenting Author: Shane Day, DO, MPH, MS, CP
CATEGORY A SCHEDULE
IN-PERSON/LIVE STREAM MEETING POSTER REVIEW / QUIZ THURSDAY, JUNE 13 Room 8:00 8:30 Opening Ceremony / Welcome: UHMS President: Pete Witucki, MD Grand Ballroom ABC 10:00 11:30 Plenary: International Panel: Diving Decompression an actual view: Costantino Balestra, Jack Kot, Jean-Pierre Imbert Grand Ballroom ABC 11:30 12:00 Posters: Session A1; A4-A6; B7-B8; E66-E67 Grand Ballroom D A4: Effective Decompression Sickness Diagnosis: Proof-of-concept Machine Learning Biomarker Selection and Predictive Modelling with Blood Transcriptome Presenting Author: Daniel Landry, MD on behalf of Jing Zhang PhD B8: Comparison of Hyperbaric Oxygen Treatment Pressures for Radiation-Induced Hemorrhagic Cystitis Presenting Author: Riggs Sanchez BA C35: Genomic Expression Patterns in Recreational Divers with Type 1 Decompression Sickness Prior to Hyperbaric Oxygen Therapy Presenting Author: Daniel Landry, MD, CCFP, DRCPSC E66: Pseudoephedrine prophylaxis does not prevent middle ear barotrauma in hyperbaric oxygen therapy Presenting Author: Kinjal Sethuraman MD MPH 14:10 14:20 A2: Reduction of inflammatory mediators and neutrophil activation by hyperbaric oxygen in patients with decompression sickness or carbon monoxide poisoning: Stephen Thom, MD, PhD Grand ballroom ABC 14:20 14:30 A3: Pressure-related inflammatory responses of SCUBA divers and tunnel workers: Phi-Nga Jeannie Le, MD Grand ballroom ABC 14:30 15:00 Plenary: UHM Fellows: Top Articles in Hyperbaric Medicine: Emma Rogers, MD: UPenn Fellow Grand ballroom ABC 16:40 16:50 B8: Comparison of Hyperbaric Oxygen Treatment Pressures for Radiation-Induced Hemorrhagic Cystitis: Riggs Sanchez, BA Grand ballroom ABC 17:00 17:30 Posters: Session B10 - B25; B27 - B33 Grand Ballroom D B15: Frequency of Urgent Consults for Hyperbaric Oxygen Therapy Presenting Author: Kinjal N Sethuraman, MD, MPH B25: A Systematic Review of Iatrogenic Air Gas Embolisms Presenting Author: Benito Pascua, MD B29: Reducing incidence of PE tube placement Presenting Author: Jennifer Wright, CHRN, BSN B30: Assessment of Prevention of Middle Ear Barotrauma in Clinical Hyperbaric Facilities Presenting Author: Jayesh B. Shah, MD B31: A Physiological Model for DCS Presentations Presenting Author: Michael B. Strauss MD B33: Text Alert Notifications and Care Process Model Used to Increase Hyperbaric Consultation Rate for Carbon Monoxide Poisoning Presenting Author: Marc Robins, DO, MPH FRIDAY, JUNE 14 9:00 10:00 Plenary: Principles of isobaric counter diffusion to prevent DCS: Richard Moon, MD Grand Ballroom ABC 10:30 10:40 C34: First-in-human imaging of venous gas emboli using a capacitive micromachined transducer toward an underwater wearable ultrasound for personalized decompression: Virginie Papadopoulou, PhD Grand Ballroom ABC 10:40 10:50 C108: Innate immune cell responses from elevated pressures and dissolved gases using human lung-on-a-chip devices: Abigail Harrell Grand Ballroom ABC 10:50 11:00 C36: Decompression stops at three instead of six meters of sea water could reduce the risk of decompression sickness: Oscar Plogmark, MD Grand Ballroom ABC 11:30 12:00 Posters: Session C34 - C39 Grand Ballroom D C34: First-in-human imaging of venous gas emboli using a capacitive micromachined transducer toward an underwater wearable ultrasound for personalized decompression Presenting Author: Virginie Papadopoulou, PhD C36: Decompression stops at three instead of six meters of sea water could reduce the risk of decompression sickness Presenting Author: Oscar Plogmark,MD C38: Decompression Gas Bubble Dynamics in the Spinal Cord of Live Rats Presenting Author: Jens-Christian Meiners C39: Midpoint assessment: A prospective trial on intra- and inter-subject variability in venous gas emboli and other biomarkers after repeated dives. Presenting Author: Joshua Currens, BS C108: Innate Immune Cell Responses from Elevated Pressures and Dissolved Gases using Human Lung-on-a-chip Devices Presenting Author: Abigail Harrell 15:00 15:10 D40: Effect of BHB level and Gender on Latency to CNSOT: Bruce J. Derrick, MD Grand Ballroom ABC 15:20 15:30 D42: Dive profiles and DCS rate among seafood harvesters in British Columbia Canada: Sherri Ferguson, MSc Grand Ballroom ABC 16:00 16:30 Plenary: UHM Fellows: Top articles in Undersea Medicine: Thomas Gregory, MD: Duke Fellow Grand Ballroom ABC 17:00 17:30 Posters: Session D40 - D57 & D59 Grand Ballroom D D40: Effect of BHB level and Gender on Latency to CNSOT Presenting Author: Bruce J. Derrick, MD D42: Dive profiles and DCS rate among seafood harvesters in British Columbia Canada Presenting Author: Sherri Ferguson MSc. D45: Cutaneous Decompression Sickness in Cozumel Presenting Author: Montserrat May Araujo MD D48: Selection of Pre-Dive Ketone Regimen to Evaluate Impact of Short-Term Ketosis on Latency to CNS O2 Toxicity in Working Divers (KETOX 2) Presenting Author: Kreager Taber, BA D49: New methods for head out water immersion in freely behaving rats to study CNS oxygen toxicity Presenting Author: Courtney Wheelock, PHD D53: Recovery from pulmonary oxygen toxicity: a new (ESOT) model Presenting Author: Jan Risberg, MD, PhD D54: Efficacy of Hyperbaric Oxygen Therapy in Cases of Decompression Sickness with Delay to Evaluation Presenting Author: Thomas J. Gregory, MD SATURDAY, JUNE 15 8:00 9:00 Davis Keynote: Non-compliant chambers: Individual liability, and a threat to our industry: Francois Burman, Pr Eng, BSc (Eng), MSc Grand Ballroom ABC 10:30 11:00 Plenary: Shortage of 24/7 Facilities: Jim Chimiak, MD Grand Ballroom ABC 11:00 11:15 Plenary: Mass CO poisoning: Geness Koumandakis, CHT Grand Ballroom ABC 11:15 12:15 Plenary: DCI treatment debate: Shorter oxygen exposures vs US Navy treatment tables: TBD (Pros) & Richard Moon, MD (Cons) Grand Ballroom ABC 12:15 13:00 Plenary: Tech's going off the reservation: Upholding the CHT Code of Conduct: Grand Ballroom ABC 14:00 14:30 Plenary: Session E: Monoplace hyperbaric chamber, equipment for treating critically ill patients: Lin Weaver, MD Grand Ballroom ABC 14:40 14:50 E61-62: Continuous blood glucose monitor performance in a 100% hyperbaric oxygen environment & Continuous blood glucose monitors and safety in the hyperbaric environment: Enoch Huang, MD & Jacquline Hocking, CHT Grand Ballroom ABC 14:50 15:00 E63: 3D Printed IV Pass Through for Monoplace Hyperbaric Chambers: Jeffrey Cooper, MD Grand Ballroom ABC 15:00 15:30 Posters: Session E60-E65, E68, E70-E72; F73-F74; F76-F83 Grand Ballroom ABC E61: Continuous blood glucose monitor performance in a 100% hyperbaric oxygen environment Presenting Author: Enoch Huang, MD E62: Continuous blood glucose monitors and safety in the hyperbaric environment Presenting Author: Jacquline Hocking, CHT E63: 3D Printed IV Pass Through for Monoplace Hyperbaric Chambers Presenting Author: Erin Etoll-Jones, MD; Jeffrey Cooper, MD E64: Delivering Hyperbaric Oxygen in the COVID-19 Era: The effect of eliminating air breaks on incidence of oxygen toxicity seizure Presenting Author: Abigail Winn MD E70: POCUS in the Multiplace Chamber Presenting Author: Christian Repollet Otero E72: Operational and patient characteristics of a new, hospital-based hyperbaric facility Presenting Author: Troy Madsen, MD F78: A Case Series of 5 Patients with pneumothorax successfully treated with HBO without tube thoracostomy Presenting Author: Abigail Winn MD F79: Cold Urticaria Preventing Clearance For Scientific Diving Presenting Author: Dan Popa, MD PhD F80: A mysterious CAGE and the man inside Presenting Author: Natalie Ouellette BSc MD F81: Respiratory Decompensation during Hyperbaric Oxygen Therapy in a patient with Severe Aortic Stenosis Presenting Author: Christopher Allen, MD F83: Position change during hyperbaric oxygen therapy for arterial gas embolism Presenting Author: Naoto Jingami, MD, PhD 16:30 17:00 Posters: Session F: 84 - F107 Grand Ballroom D F85: Fulminant decompression illness in a recreational diver without significant omitted decompression. Presenting Author: Laura M. Lauer, DO F101: Safety of delivering Hyperbaric Oxygen therapy in a patient with Lung transplant: a case report Presenting Author: Jayanth Adusumalli MBBS, MPH F104: Alcohol intoxication vs decompression sickness Presenting Author: Christopher Leiker, M.D. F105: Patient Suffering Guillain Barré Syndrome Mimicking Neurological Decompression Syndrome Presenting Author: Richard Fontanez, Pedro Arroyo - NBDHMT:This live activity is approved for a maximum of 20* Category A credit hours by National Board of Diving and Hyperbaric Medical Technology, P.O. Box 758, Pelion, South Carolina 29123. *Up to 15 Cat A credits for the in-person/live stream meeting and up to 5 Cat A credits for reviewing posters/quiz online at your leisure. Not to exceed 20 total maximum Cat A credit hours.
