Standards and Codes
I have 3 hyperbaric chambers. The facility is storing wound care supplies in my chamber area and all throughout the day they walk back and forth through there to get supplies. Clearance from the chamber doors are about 10-12 feet and they walk directly behind them. NFPA 99 says the room housing the chambers should be for hyperbarics exclusively. My facility wants guidelines on if I have room to load the chambers then can they still store their supplies back there and walk through there throughout the day.
Posted: 2/10/25
Q:
I have three (3) hyperbaric chambers. The facility stores wound care supplies in my chamber area, and throughout the day, they walk back and forth to get supplies. Clearance from the chamber doors is about 10-12 feet, and they walk directly behind them. NFPA 99 says the room housing the chambers should be exclusively for hyperbarics. My facility wants guidelines on whether I have room to load the chambers, and if they can still store their supplies back there and walk through them throughout the day. Total clearance from the chamber doors is only 12 feet. Not to mention the hazard of having people walk through the facility all day while I try to treat patients. Can you give me anything useful so I can get my facility to move their wound care supplies to the wound care clinic?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
Regarding NFPA codes, since the Centers for Medicare and Medicaid Services cite the 2012 edition (which means The Joint Commission and DNV must cite, too), we have included references to that addition and the most recently published edition of 2024.
It is important to note that NFPA 99 hyperbaric fire and safety codes place the responsibility of enforcement on the facility Governing Board (leadership) and the Hyperbaric Safety Coordinator/Director (NFPA 99, 2012 & 2024 eds., 14.3 Administration and Management).
As you stated, NFPA codes state: When used for hyperbaric procedures, the room or rooms housing the Class A or Class B chambers shall be for the exclusive use of the hyperbaric operation (NFPA 99, 2012 & 2024 eds., 14.2.1.1.7). The UHMS Safety Committee cannot formally interpret NFPA codes, but we can provide our thoughts regarding your situation.
If The Joint Commission accredits your hospital, we recommend you meet with your accreditation team and review the Hyperbaric Oxygen Chamber Compliance Checklist, precisely page 5, where the following question is asked: Does the organization ensure that any room used for hyperbaric oxygen chambers (Class A or B) is not used for any other purpose (Joint Commission Resources)?
It is important to remember that the room housing your hyperbaric chambers is designed to provide medical treatment – therefore, it is a medical treatment room and not a storage closet. Some of the same reasons a facility would not store extra supplies in an exam room apply to not storing them in a hyperbaric treatment room.
Concepts of Hazard Avoidance
A hazardous situation involves risk and chance. The most effective way to prevent a hazard is elimination. The process of hazard elimination, regarding your situation, is to limit access and travel in and out of the hyperbaric treatment room for the following reasons:
- Limit distractions – the focus of the chamber operators must be on the hyperbaric patients and not be distracted by staff entering and exiting the room for issues unrelated to hyperbaric therapy.
- Complacency – when the hyperbaric treatment room is approached casually, you establish a complacency behavior, a “what does it matter” mentality, which leads to mistakes and accidents.
- Storage Drift – when using the hyperbaric room to store non-hyperbaric related items (in this case, wound care supplies), drift may occur where items other than wound care start to appear, such as paint, chemicals, floor cleaners, etc.
- Patient privacy – the only staff that needs to be in a treatment room are those treating the patients.
- Cleanliness – the more people that enter and leave the hyperbaric treatment room, the less clean the room will remain.
- Operations – when non-essential staff are in the hyperbaric room, there is an increased risk of impeding normal operations.
Respectfully,
UHMS HBO2 Safety Committee
References:
Joint Commission Resources. (2021). Hyperbaric oxygen chamber compliance checklist. Environment of Care News. February 2021.
NFPA 99. (2011). NFPA 99 Health care facilities code (2012 ed.). National Fire Protection Association.
NFPA 99. (2023). NFPA 99 Health care facilities code (2024 ed.). National Fire Protection Association.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice
Could you please tell me the industry recommendation for how many people must be present to run monoplace hbo chambers. If running 2-3 chambers, do we need 2 or 3 people present? I understand we need an operator and provider to supervise, do we need a 3rd person or can the provider also serve as a 2nd operator as well?
Posted: 10/16/24
Q: Could you please tell me the industry recommendation for how many people must be present to run monoplace hbo chambers. If running 2-3 chambers, do we need 2 or 3 people present? I understand we need an operator and provider to supervise, do we need a 3rd person or can the provider also serve as a 2nd operator as well?
A: You can purchase the document here - Best Publishing Company - UHMS Guidelines for Hyperbaric Facility Operations 3rd Edition.
Q: That is helpful, however, if operating 3 chambers, is the second operator able to be the provider or should this be a 3rd person?
A: If you have three chambers with patients under pressure, you need two staff members to see the treatment. The second person can be a provider if they stay chamber side and not string to see patients simultaneously.
Derall Garrett, CHT-A
Hyperbaric Facility Accreditation Director
Is there a requirement for accreditation to have documentation of a yearly check of each monoplace chamber that includes a staff member inside at treatment pressure to verify the function of the air break system?
Posted: 4/18/2024
Q: Is there a requirement for accreditation to have documentation of a yearly check of each monoplace chamber that includes a staff member inside at treatment pressure to verify the function of the air break system?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/C) of your facility.
The UHMS Accreditation manual identifies in section HBOV 2.3 that:
“The proper function of individual breathing apparatus at all pressures that can be encountered in the chamber has been documented. This applies to Class A multiplace chambers and Class B monoplace chambers with air break capability.”
The UHMS HFA Accreditation manual does not require an annual test of the apparatus by a staff member. This section of the UHMS accreditation manual is derived from NFPA 99, Chapter 14, section 14.2.4.1.3.3 (multiplace) and 14.2.4.4.3 (monoplace):
14.2.4.1.3.4: “Breathing apparatus shall function at all pressures that can be encountered in the chamber.”
14.2.4.4.3: “For Class B chambers equipped with a breathing apparatus, the breathing apparatus shall function at all pressures that can be encountered in the chamber.
This language was originally introduced into NFPA code pertaining to multiplace hyperbaric chambers that require each occupant to have a breathing apparatus in case the chamber atmosphere became fouled. As the industry shifted to a majority of monoplace chambers, the code language was adopted for class B chambers. Simply put, the NFPA does not mandate exactly how to meet this section of code, nor how frequently this is to be done. This should be determined by the manufacturer and based upon the type of equipment used.
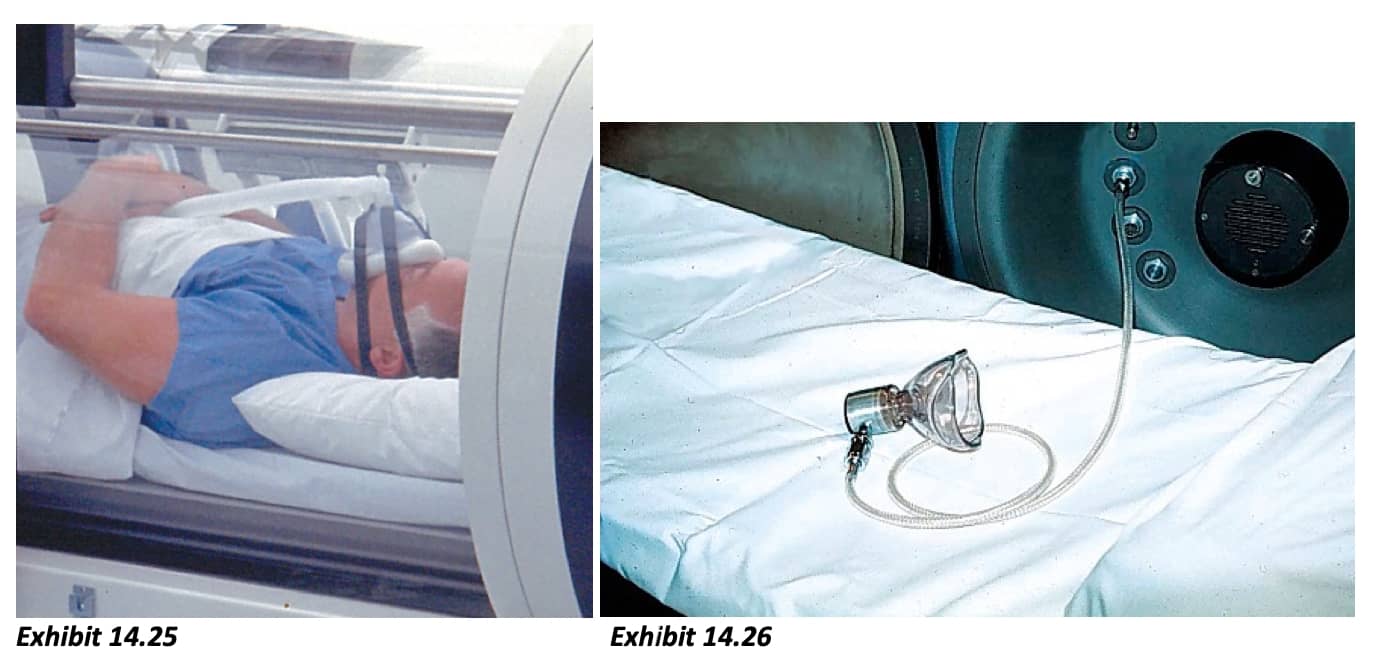
There are many different types of air break masks or breathing apparatus employed in hyperbaric facilities. Examples of these masks are shown in the NFPA 99 Handbook. (exhibits 14.25, 14.26, 14.27)
Some facilities utilize a free-flow design, and others use a demand-style. It is important to make this distinction because these masks can be used for either air or oxygen delivery, and there may be a limit to the gas supply pressure at which the apparatus can function properly.
There are many facilities who use non-rebreather masks (NRBs) for air breaks. These types of masks are not generally thought of as a breathing apparatus, as this was not the type of device used in chambers to meet this code when the language was first used. However, it is reasonable to suggest that a NRB should function normally at all pressures, provided that sufficient gas supply pressure is present. Many Class B chamber facilities choose to implement a daily or weekly verification of free-flow function of the NRB, typically by viewing the reservoir bag inflate at pressure.

As it pertains to breathing apparatus containing a demand valve, the testing of these devices is most likely to have occurred during installation by the manufacturer, who would suggest the frequency of testing for preventative maintenance purposes. This can be done either by the manufacturer or a qualified person.
If documentation of testing upon installation does not exist for a breathing apparatus containing a demand valve, the UHMS Safety Committee recommends that this be performed with input from the manufacturer. This can be done by the manufacturer but is often completed by hyperbaric staff with guidance from the manufacturer. Within your testing documentation, we suggest including the manufacturer’s data, initial installation date, maintenance and test documentation, any formal testing and published test results for a given apparatus. This approach could also apply to Class A Multiplace facilities.
Respectfully,
UHMS HBO2 Safety Committee
BIBLIOGRAPHY:
- NFPA 99. (2023). NFPA 99 Heath care facilities code (2024 ed.) National Fire Protection Association.
- Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.) Undersea and Hyperbaric Medical Society, Inc.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and hyperbaric safety director/coordinator of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We did our yearly hospital wide fire drill the other day with officers from our local fire dept observing. We did a fire inside the chamber and one of the observations was that the heat build up inside the chamber would make it impossible for someone to remove the stretcher without protection on their hands. Another suggestions was to have an emergency electrical shut off switch by the chamber to cut off any electricity to the chamber for when the sprinkler system activates. They also recommended a Class
Posted: 2/1/2024
Q: We did our yearly hospital wide fire drill the other day with officers from our local fire dept observing. We did a fire inside the chamber and one of the observations was that the heat build up inside the chamber would make it impossible for someone to remove the stretcher without protection on their hands. Another suggestions was to have an emergency electrical shut off switch by the chamber to cut off any electricity to the chamber for when the sprinkler system activates. They also recommended a Class C fire extinguisher for any type of electrical fire in the chamber room. I was wondering if you have heard about any of these suggestions or anything similiar. Thank you.
A:
My name is Andrew Melnyczenko, Chair of the UHMS Hyperbaric Safety Committee, and your question was forwarded to me by John Peters, Executive Director of the UHMS. I'm happy to assist you in answering your question but please keep in mind that the ultimate responsibility for these decisions rests upon the Hyperbaric Safety Director, and Hyperbaric Medical Director of your program.
1. The NFPA 99 does not address personal protective equipment in the setting of a hyperbaric fire, outside of protective respiratory equipment and emergency breathing. Fortunately, NFPA 99 is currently in an open comment cycle. I would encourage you to bring this to the attention of the NFPA by submitting a public comment on this topic. https://www.nfpa.org/customer-support/how-do-i-submit-a-public-comment-on-an-nfpa-standard
2. NFPA 99 does contain a requirement for Class 'A' hyperbaric chamber systems to have the ability de-energize circuitry entering the chamber in the event of a fire. In many instances, chamber Fire Suppression Systems cut power to these circuits as the deluge system is activated: 14.3.4.4.1.2 In the event of fire, all nonessential electrical equipment within the chamber shall be de-energized before extinguishing the fire. (A) Smoldering, burning electrical equipment shall be de-energized before extinguishing a localized fire involving only the equipment. (See 14.2.6.) 3. NFPA 99 does not specify the type of fire extinguisher to be utilized outside of the chamber. This is a decision that is typically made by the local authority having jurisdiction (AHJ).
I hope this information is helpful to you Sir, please do not hesitate to contact me if you have any further questions.
Sincerely, Andrew Melnyczenko, CHT
We will be due for our yearly PM in January. we had our acrylics inspected last year, was wondering if that has to be inspected yearly or every 2 years.
Posted: 12/8/23
Q: We will be due for our yearly PM in January. we had our acrylics inspected last year, was wondering if that has to be inspected yearly or every 2 years.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director/Coordinator (HSD/HSC) of your facility.
- The frequency of the maintenance viewport inspection is dependent on service environment, , age, cycles, and design life of the acrylic.
- For protected environment (typical for hospital and clinic-based facilities), inspection should occur every 36 months during design life, and then every 24 months after an extension until 20 years.
- For severe environments the inspection cycle is more frequent. (See definition below).
- Facilities may always choose to exceed the standard. This is not required, but it is somewhat common.
From: (2019) ASME PVHO-2, Table 2-4.3-1 Maximum Intervals for Maintenance Viewport Inspection:
|
Actual Service Duration and/or Cycles |
Protected |
Typical |
Severe Service |
|
Less than design life Greater than design life |
36 months 24 months |
24 months 18 months |
18 months 12 months |
|
General Notes: a) Window removal is not required unless deemed necessary by the inspector. b) Because of the critical adjustments of tie rods, cylindrical window chambers should not normally be disassembled on a periodic basis for performance of maintenance viewport inspections |
|||
Here are some helpful definitions that may provide you with some clarity:
From (2019) ASME-PVHO-2:
protected environment: benign conditions consisting of controlled ambient temperature and minimal exposure to UV radiation, chemicals, and abrasion, that the designer would expect to have minimal effect on the service life of the window (medical chambers are typically operated in a protected environment).
PVHO Window Design Life: The length of time as defined by para. 2-2.7 of ASME PVHO-1 that the designer uses for a particular geometry window.
severe environment: any conditions of temperature extremes, pressure, radiation (i.e., UV light), and pressurization medium or contamination that the designer would anticipate to shorten the service life of the window (marine systems are typically, but not necessarily, operated in a severe environment).
From (2019) PVHO-1:
design life (windows): the period of time and/or number of design cycles assumed for a window complying with this Standard. The window design life may be different for different types of windows. The design life has three aspects: total time under pressure, cycle design life, and total chronological time from the date of initial manufacture.
For your convenience, we would also like to share a fillable PDF inspection form, created by one of our members. This form was duplicated from page 19 of the 2019 ASME PVHO-2 In-Service Guidelines (copying is allowable by ASME-PVHO). This document may assist you in completing the maintenance inspection. We encourage you to complete and retain form VM-1 with each viewport inspection.
As stated in ASME PVHO-2-2019, Section 1 General, 1-4 PVHO and PVHO systems documentation:
The owner shall be responsible for maintaining the following documentation for the service life of the PVHO and PVHO systems:
(a) documentation required by ASME PVHO-1, section 1, General Requirements
(b) documentation generated during inspection, maintenance, repairs, and modifications
(c) documentation related to operational procedures and manuals
Notes pertaining to the user and inspector:
- The user assigned to establish and maintain the facility’s viewport inspection program should be familiar with the full content of ASME PVHO-2 section 2 Viewports.
- The user is responsible for determining that a window inspector, whether internal or a third-party employee, has met the appropriate inspector’s level of qualification as stated in ASME PVHO-2.
- The level of qualification is typically different for the Operational Viewport Inspection Inspector vs the Maintenance Viewport Inspection Inspector.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Davison W, “Establishing a Viewport Inspection Program: What to Know,” Published in PRESSURE, Undersea and Hyperbaric Medical Society, 2021 https://www.uhms.org/publications/pressure/fourth-quarter-pressure-2021/viewdocument/4882.html
- MEDFAQ Response, “Inspection requirements for a monoplace chamber,” Published 3/16/15 https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/160-standards-and-codes.html?faq=3<
- The American Society of Mechanical Engineers. (2019). ASME PVHO-1-2019: Safety Standard for Pressure Vessels for Human Occupancy. Two Park Avenue, New York, NY
- The American Society of Mechanical Engineers. (2019). ASME PVHO-2-2019: Safety Standard for Pressure Vessels for Human Occupancy. Two Park Avenue, New York, NY
ASME PVHO 2-2019 PVHO-2 Form VM-1 Viewport Inspection Report
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Are there any potential hazards or contraindications from running the chambers if the hyperbaric room temperature is higher than normal (higher than room temperature)? For example, if the air conditioning system fails in the room on a summer day.
Posted: 8/28/2023
Q:
Are there any potential hazards or contraindications from running the chambers if the hyperbaric room temperature is higher than normal (higher than room temperature)? For example, if the air conditioning system fails in the room on a summer day.
A:
Thank you for your question concerning the ambient temperature in the room where monoplace hyperbaric operations are taking place. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The Sechrist Installation Requirements and Technical Instruction Guide cites a “Temperature Range” between 50°F and 100°F on page 4-1 “Equipment Specifications.” This refers the internal operating temperature of the chamber, which can also be impacted by the room temperature. Additionally, on page 2-3 within the “Hyperbaric Facility Requirements” section, Sechrist recommends that the “Temperature in the room (housing the chamber) should be maintained in the range of 68 – 74 degrees Fahrenheit for patient comfort.”
Based upon the manufacturer’s suggestions, we suggest that you follow these instructions. Colder temperatures (below 50°F) may impact the chamber’s seat and seal, perhaps leading to chamber leakage. Higher temperatures (>100F) will take the acrylic beyond its designed operating parameters and would be quite uncomfortable for the patient.
Additionally, the building’s HVAC systems effect the ability to control humidity and temperature, which can impact the control of static electricity within the chamber room. Increased temperature also effects the ability to provide comfort to chamber operators, as they may not be able to concentrate and work effectively under these extreme conditions.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc. LINK
- Sechrist Industries, Inc., “Sechrist Installation Requirements and Technical Instruction Guide.” Rev. 6, Anaheim, CA
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Does the UHMS have a position on whether a patient in a HBOT chamber is considered ambulatory or non-ambulatory during the treatment period? The definition has impacts on the oxygen service for clinics.
Posted: 7/10/2023
Q:
Does the UHMS have a position on whether a patient in a HBOT chamber is considered ambulatory or non-ambulatory during the treatment period? The definition has impacts on the oxygen service for clinics.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The definitions found in the 2018 editions of NFPA 99 and NFPA 101 that were offered as a reference to your question are listed below. The 2021 version of these sections of code have not changed. Certain accreditation standards may reference older versions of NFPA 101 and 99.
NFPA-99, 2018 Edition, Chapter 3: Definitions
3.3.5 Ambulatory Health Care Occupancy.
An occupancy used to provide services or treatment simultaneously to four or more patients that provides, on an outpatient basis, one or more of the following: (1) treatment for patients that renders the patients incapable of taking action for self-preservation under emergency conditions without the assistance of others; (2) anesthesia that renders the patients incapable of taking action for self-preservation under emergency conditions without the assistance of others; (3) treatment for patients who, due to the nature of their injury or illness, are incapable of taking action for self-preservation under emergency conditions without the assistance of others. [101, 2018] (FUN)
NFPA-101, 2018 Edition, Chapter 3: Definitions
3.3.196.1 * Ambulatory Health Care Occupancy.
An occupancy used to provide services or treatment simultaneously to four or more patients that provides, on an outpatient basis, one or more of the following: (1) treatment for patients that renders the patients incapable of taking action for self-preservation under emergency conditions without the assistance of others; (2) anesthesia that renders the patients incapable of taking action for self-preservation under emergency conditions without the assistance of others; (3) treatment for patients who, due to the nature of their injury or illness, are incapable of taking action for self-preservation under emergency conditions without the assistance of others. (SAF-HEA)
A.3.3.196.1 Ambulatory Health Care Occupancy.
It is not the intent that occupants be considered to be incapable of self-preservation just because they are in a wheelchair or use assistive walking devices, such as a cane, a walker, or crutches. Rather, it is the intent to address treatment centers that receive patients who have been rendered incapable of self-preservation, such as being rendered unconscious as a result of an accident or being unable to move due to sudden illness. It is not the intent that the term anesthesia be limited to general anesthesia.
Regarding the means of egress during any operation involving a patient inside of a hyperbaric chamber, it is the view of the UHMS HBO2 Safety Committee that the patient does not have the capability to remove themselves from a dangerous situation. Both the Class A Multiplace and Class B Monoplace hyperbaric chamber require training to operate. The person inside cannot immediately egress the room housing the chamber without outside assistance. This fact alone is the determining factor in our assessment of this text.
As stated in (2018) NFPA 99 3.3.5:
(1) treatment for patients that renders the patients incapable of taking action for self-preservation under emergency conditions without the assistance of others;
(and)
(3) treatment for patients who, due to the nature of their injury or illness, are incapable of taking action for self-preservation under emergency conditions without the assistance of others.
Additionally, if internal chamber controls exist, the UHMS HBO2 Safety Committee does not recommend the training of patients to decompress themselves in the event of an emergency. NFPA Chapter 14 addresses the need for external chamber operators:
(2018 and 2021) NFPA 99: 14.3.1.4.6 During chamber operations with an occupant(s) in a chamber, the operator shall be physically present and shall maintain visual or audible contact with the control panel or the chamber occupant(s).
A.14.3.1.4.6 The complexity of hyperbaric chambers is such that one person should be designated chamber operator, such as a person in a position of responsible authority.
Also, since Det-Norske Veritas (DNV) and the Joint Commission (TJC) currently follow the 2012 editions of NFPA 101 and 99, we suggest that the hospital should evaluate the life safety occupancy classification for the proposed Wound Care Center location based on requirements from the Life Safety Code (NFPA 101 – 2012 ed.). Because a hyperbaric patient in the chamber depends upon the actions of Wound Care Center staff in an emergency, these patients are temporarily rendered incapable of taking actions for self-preservation by the hyperbaric procedure.
If the intent is to remain in compliance with DNV and TJC, we recommend applying the requirements of either new or existing Ambulatory Healthcare Occupancies described in NFPA 101-Life Safety Code, 2012 edition. The Centers for Medicare & Medicaid Services (CMS) adopted NFPA-101; 2012 edition and NFPA-99; 2012 edition and began surveying these editions as of July 2016.
Respectfully,
The UHMS HBO2 Safety Committee
REFERENCES:
- National Fire Protection Association. (2012, 2018, 2021). NFPA 101: Life Safety Code. Quincy, Massachusetts.
- National Fire Protection Association. (2012, 2018, 2021). NFPA 99: Health Care Facilities Code. Quincy, Massachusetts.
- National Fire Protection Association. NFPA resources for CMS requirements (Accessed 7/7/2023).
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I am an active UHMS member and current medical director of an HBO facility accredited by UHMS, which is located within Portneuf Medical Center. We are planning to build a new HBO facility for 3 individual chambers. I would appreciate it if you could provide information about technical specifications on how to properly build it. Referral to architects, documents or any other valuable information is welcome. Thanks.
Posted: 1/10/23
Q:
I am an active UHMS member and current medical director of an HBO facility accredited by UHMS, which is located within Portneuf Medical Center. We are planning to build a new HBO facility for 3 individual chambers. I would appreciate it if you could provide information about technical specifications on how to properly build it. Referral to architects, documents or any other valuable information is welcome. Thanks.
A:
I’d like to share the enclosed resources with you and point you towards the Facility Guidelines Institute’s 2022 Guidelines for Design and Construction of Hospitals. (Formerly an AIA guideline) https://www.fgiguidelines.org/
The enclosed documents contain a copy of the 2006, 2010 and 2014 guidelines as references for your information, but I would encourage you to follow the most current edition.
The UHMS Hyperbaric Facility Accreditation Manual is a great resource to prepare your facility with the Best Practice standards observed by the industry. Of course, the NFPA 99 Handbook is also a great reference that every Hyperbaric Facility should own. Finally, there is an older reference - 2004 UHMS Facility Design - that may still have relevance as it rightly concludes in the opening paragraph “there is no national standard for the design of a hyperbaric facility.” Another important factor to consider is that there may be various codes and statutes enforced by Authorities Having Jurisdiction in your area which will impact design. Of note, the State of Idaho has recently released the following statement regarding the construction of hyperbaric facilities: https://doi.idaho.gov/wp-content/uploads/ID/B23-01.pdf
I hope that these resources will assist your facility and I wish you the best of luck in this worthy endeavor. Please reach out to us if you have additional questions.
Regards,
Andrew Melnyczenko, BSHCA, CHT
Technical and Safety Director – Hyperbaric and Altitude Medicine, Division of Public Health, Infectious Diseases, and Occupational Medicine
We have been grandfathered in so our clinic is still in a billable area. But if we were to move our clinic what is the distance we have to be within from the hospital.
Posted: 12/2/2022
Q: We have been grandfathered in so our clinic is still in a billable area. But if we were to move our clinic what is the distance we have to be within from the hospital.
A: 250 yards
Is there a policy for HBO treatments in single person chamber that hbo tech can monitor patients with camera monitor installed on the outside of the chambers? Can the technician leave the HBO room with the monitor?
Posted: 3/7/22
Q:
Is there a policy for HBO treatments in single person chamber that hbo tech can monitor patients with camera monitor installed on the outside of the chambers? Can the technician leave the hbo room with the monitor?
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility.
The UHMS HBO2 Safety Committee appreciates your attention to the guidelines and standards that have been established for the hyperbaric community. It is important to note that the NFPA 99 (2021), 14.2.1.4.2 gives joint authority to the HMD and HSD to determine the “minimum staff qualifications, experience, and complement based on the following:
(1) Number and type of hyperbaric chambers in use
(2) Maximum treatment capacity
(3) Type of hyperbaric therapy normally provided”
As such, the UHMS HBO2 Safety Committee recommends that a written policy is developed by the HMD and HSD that identifies the staffing levels necessary for the safe delivery of hyperbaric oxygen therapy based upon the above factors, and perhaps several other considerations that may be unique to your particular program.
The Safety Committee identifies several reasons why leaving a chamber unmanned would be deemed unsafe:
- It is important to consider the chamber operator’s ability to respond to an emergency. Remaining outside of the chamber room watching via CCTV will severely limit your ability to respond to the patient.
- There is likely no way for the patient to effectively communicate to the staff.
- Be aware that screens are two-dimensional and is not an optimal way to discern visual depth. For example, it may be difficult to visualize facial twitching, a symptom of oxygen toxicity.
- If sound is used, filtering out the noise of the ventilation system would be necessary.
- It is also important to consider that the patient would feel totally alone and unattended. Ask yourself, is it reasonable to leave a patient alone in a room, laying inside a sealed chamber for over an hour? Would you ever leave a patient alone for this long otherwise?
- The potential for the observer to be distracted and/or have their attention divided outside of the chamber room is highly likely (the whole purpose of being outside the chamber room is to be able to multitask), and the temptation to visit the bathroom or elsewhere hence leaving the screen unmanned is too high
Referenced Staffing Considerations:
- The NFPA 99 Health Care Facilities Code, 2021 edition, 14.3.1.4.6 requires that:
“During chamber operations with an occupant(s) in a chamber, the operator shall be physically present and shall maintain visual or audible contact with the control panel or the chamber occupant(s).”
- The NFPA 99 Handbook also adds this note:
“It is vitally important that a qualified chamber operator be present during chamber operations. The number of qualified chamber operators required will vary depending on the type of chamber(s), number of chambers being operated simultaneously, number and acuity of the patients, qualifications of the hyperbaric staff. and layout of the room housing the chambers. The chamber operator should always have someone available to call for help in an emergency or to provide breaks.”
- The UHMS HBO2 Safety Committee agrees with the following staffing guidelines provided in “UHMS Guidelines for Hyperbaric Facility Operations, 2nd ed.,” as it relates to Monoplace facilities:
Section 3, Staffing Guidelines (pg.15):
“One (1) chamber operator should not operate and/or monitor more than two (2) monoplace chambers simultaneously during patient treatments”
“At least one (1) additional hyperbaric-trained staff member should be immediately available to assist, if needed, during any patient treatment.”
- The Baromedical Nurses Association also supports the UHMS’s staffing guidelines for monoplace operations within a hyperbaric facility.
- Ensure that the Hyperbaric Safety Director is working closely with the Hyperbaric Medical Director to establish the minimum complement of staff as indicated in the UHMS Clinical Hyperbaric Facility Accreditation Manual, UHMS Guidelines for Hyperbaric Facility Operations, 2nd ed., and NFPA 99 14.3.1.4.2.
The existing MEDFAQs https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq/safety-technical/160-standards-and-codes.html, refers to the UHMS Hyperbaric Facility Operations Guidelines, Section 3, Staffing Guidelines.
Specifically, Part III, Hyperbaric Technician/Chamber Operations Staff, bullet one, states a minimum of one CHT, CHRN or CHS should be on duty in the clinical area when a patient is receiving treatment. It doesn’t appear there is any exception or allowance to be monitoring by video and not in the clinical area.
In closing, we encourage administrators and program managers responsible for the safety of their hyperbaric programs to consider the standards and recommendations we have listed here and allow staffing decisions such as these to be made jointly by the HMD and HSD of the hyperbaric program. We also suggest that the HMD and HSD conduct a formal Risk Assessment that is inclusive of the factors mentioned above prior to developing a staffing policy for the program. We understand that there may be many other considerations not mentioned here that are unique to your facility and should be included within the risk assessment.
REFERENCES:
UHMS HBO2 Safety Committee response to MEDFAQ, Accessed 9/28/2020, Originally published 2/23/2017.
Workman, W. T. (2015). Guidelines for Hyperbaric Facility Operations (2nd ed.). North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc.
National Fire Protection Agency (NFPA). (2018). NFPA 99 2018 Edition: Health Care Facilities Code. Quincy, Massachusetts.
Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.). North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Hi there, I was wondering why water-only fire extinguishers are used in hyperbaric suites with monoplace chambers and not ABC fire extinguishers? It seems like anywhere that you might have an electrical fire source, it would be a good idea to have a chemical type of extinguisher. Is water-only a standard when it comes to monoplace chambers? Thank you very much.
Posted: 3/3/22
Q:
Hi there, I was wondering why water-only fire extinguishers are used in hyperbaric suites with monoplace chambers and not ABC fire extinguishers? It seems like anywhere that you might have an electrical fire source, it would be a good idea to have a chemical type of extinguisher. Is water-only a standard when it comes to monoplace chambers? Thank you very much.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Hyperbaric Medical Director (HMD) and Hyperbaric Safety Director (HSD) of your facility. It is important for your HSD to be aware of the specific needs of your facility, and we applaud you for being thoughtful about your team’s ability to extinguish a fire, should the need ever arise.
The UHMS HBO2 Safety Committee is not aware of a specific code requirement for water-filled extinguishers near Monoplace chambers. However, there is no penalty for achieving a standard above the existing code. It is possible that this may have been added in your area intentionally - as some water-mist extinguishers have several features that may make it advantageous for the Monoplace suite. Certain types of water-mist extinguishers are suitable for both class A and C fires, leave zero residue, and use de-ionized water which can protect the user from electrical shock.
As you identified, most water-filled extinguishers are not suitable for Class C fires. The NFPA 99 Health Care Facilities Code, Chapter 14 (2018 and 2021 editions) contain the minimum standards for the room housing a Class A, Class B, or Class C chamber (14.2.1.2.2). The code calls for a ABC-type extinguisher. Specifically, a minimum of one 2-A:10B:C portable fire extinguisher.
In CFR 1910.157 – Portable Fire Extinguishers, the Occupational Safety and Health Administration (OSHA) addresses the requirements of “…placement, use, maintenance, and testing of portable fire extinguishers provided for the use of employees.” We would advise you to review this standard and assess how it applies to your area.
As you are thinking about your assessment, you may also wish to review these notable comments from our Safety Committee Members on this topic:
- It is important to note that the chemical Monoammonium Phosphate used in the ABC extinguishers has a static affinity to monoplace chamber acrylic and is extremely abrasive. DO NOT try to even wet wipe it off - It can only be successfully flushed off with a mild detergent diluted in warm water. In addition to the ABC extinguishers, we install a 20-pound CO2 extinguisher and train staff to alarm the building and then preferentially select the water, CO2 or ABC extinguisher as appropriate. A wastepaper basket is most appropriately extinguished with water. The CO2 and ABC are overkill and can blow burning paper around the room if used too enthusiastically. I understand this may be difficult to apply as a general policy, but a good thing for Unit Safety Directors to know.
- Many years ago (about two generations, before there were any HBO codes) when I was working in the monoplace world, we always had at least two extinguishers in the chamber room. One was an ABC and the other was a water handheld extinguisher. We also had a water fire hose immediately outside the chamber room. One of our concerns at that time was, what if there is a fire in the chamber. We wanted to be able to spray the patient and area as we opened the door. We didn't think an ABC was best for that purpose.
- I suggest that one could certainly provide a water-based extinguisher (or several) in the monoplace suite. They would be useful with the type of fire we might expect inside a class B chamber...that said the code(s) requires we have at least one ABC.
In closing, we would encourage the HSD to assess the risk in your area and then work with the Facilities Management and local Fire and Life Safety representatives of your facility to make them aware of your needs. It is important to note that in accordance with the Joint Commission (TJC), many facilities adhere to an older version of the NFPA 99 (prior to 2018) which does not require an ABC extinguisher in the chamber room.
Hyperbaric facilities are unique. You may also wish to reach out to your community’s Fire Marshal to share information about your work area and to seek further guidance. It is also important to do this regularly, as the individuals in these positions change and they may not be aware of your presence. Aside from the type of extinguisher, the HSD should also ensure that extinguisher is located within an appropriate distance and that the staff is trained to use them appropriately.
REFERENCES:
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- National Fire Protection Association. (2018, 2021). NFPA 99 2018 & 2021 Edition: Health Care Facilities Code. Quincy, Massachusetts.
- Lehtola, C. J., Brown, C. M., & Becker, W. J. (2000). Portable Fire Extinguishers: OSHA Standard 1910.157. University of Florida Cooperative Extension Service, Institute of Food and Agricultural Sciences, EDIS.
- Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.). pg. 51 – HBOEC 3.0, North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc.
- Workman, W. T. (2010). Hyperbaric Facility Safety: A Practical Guide (1st ed.). pp. 402-404, Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I am currently the HBO safety director at the hospital where I am currently employed and also have my CHRN. My question is, does the safety director have to work specifically in the HBO department or could I work as an RN in a different department within the hospital and still function in the safety director role as long as i keep my credentials up to date. We have other RN's within my department who are HBO certified that could actually run the chambers and do so when I am on vacation or otherwise unable
Posted: 3/0/2021
Q:
I am currently the HBO safety director at the hospital where I am currently employed and also have my CHRN. My question is, does the safety director have to work specifically in the HBO department or could I work as an RN in a different department within the hospital and still function in the safety director role as long as i keep my credentials up to date. We have other RN's within my department who are HBO certified that could actually run the chambers and do so when I am on vacation or otherwise unable to be here.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the Medical Director (MD) and your Hospital’s Administration as it pertains to the role of the Hyperbaric Safety Director (HSD) for your facility.
The NFPA 99, Chapter 14 (2021) places a high degree of importance in the role of the HSD. The term “Safety Director” is mentioned 26 times throughout the chapter and Appendix A. We suggest that perhaps the most relevant reference to your question is NFPA 99 14.3.1.3.2 (2021):
“Each hyperbaric facility shall designate an on-site hyperbaric safety director to be in charge of all hyperbaric equipment and the operational safety requirements of this chapter.”
The NFPA 99 Handbook provides more insight, including this Frequently Asked Question and answer. The NFPA Handbook is a separate document containing guidance for the codebook, and the FAQ sections are intended to clarify the code for the reader. The FAQ answer is not considered part of the code.
Q: “Does the on-site safety director have to be present during chamber operations?”
A: “The designated on-site safety director does not have to be present during all chamber operations. The intent is that someone manages the operational responsibilities of this chapter; this does not mean that that person must be present at all times. It is recommended that there be an alternate designee trained for succession as the hyperbaric safety director.”
While the UHMS HBO2 Safety Committee cannot determine the best approach for your situation, we can offer several considerations and recommendations that may assist your MD and Hospital Administration in this decision-making process regarding the proximity or accessibility of the HSD.
- If the HSD is working in another area, will he/she be available to respond promptly to the needs of the team if a decision is needed? What safeguards or plans exist if the Safety Director cannot be reached?
- Has an individual been assigned to assume this role in the absence of the current HSD? If so, what is the level of experience and training that person has received? Has this assignment been made in writing?
- What is the confidence level of your chamber operators in this approach to coverage? Are they willing to accept an increased level of responsibility if they are called upon to be the alternate designee?
- Have you considered sending your chamber operators to HSD courses?
- It is recommended that in a busy hyperbaric facility, an appropriately trained HSD or their designee is present in the suite and available to make day-to-day decisions. This is similar in design to the role of the supervising hyperbaric provider.
- Many multi-center monoplace-only programs operate with a regional, more experienced remote HSD, and place designated HSDs at each satellite facility, (usually an experienced CHT or CHRN). These individuals are responsible for the day-to-day decisions. The multi-site HSD remains available to provide support to each on-site HSD and may sometimes fill-in for local personnel in their absence. All these individuals typically receive additional HSD training.
- If the HSD is absent, on vacation, or sick, an appropriately trained alternate should be designated.
- The individual covering for the HSD should preferably have attended an HSD training course, have knowledge and experience in hyperbaric medicine and with the equipment used at the facility.
- As mentioned in the UHMS Guidelines for Hyperbaric Facility Operations, The Medical Director (MD) should not be the primary HSD. However, due to their appointment and level of responsibility, you may wish to consider delegating the HSD role to the MD in the absence of the HSD. In this instance we also recommend that the MD attends an HSD training course.
- There is reason to be concerned about disengagement or drift. Over time, it is likely that an individual serving from afar may become less involved with the HBO unit. Therefore, it would be advisable to have strict guidelines for the HSD, such as:
- The HSD should visit the HBO Unit (insert a frequency) and keep a log of the visits.
- The HSD should be available by phone whenever the HBO Unit calls.
- The HSD should institute a training program for chamber operators on the role and responsibilities of the HSD as outlined by the NFPA (at a minimum).
In conclusion, the UHMS HBO2 Safety Committee recommends that the Hyperbaric Medical Director, HSD and Hospital Administration examine the risks and benefits of each approach and consider the safety measures described above. We also recommend that the facility develop standardized protocols for the hyperbaric staff who will work with the HSD. There may be the need to gather recommendations from your Legal and Human Resource teams before engaging in this practice.
References
- Burman, F. (2019). Risk Assessment Guide for Installation and Operation of Clinical Hyperbaric Facilities (6th ed.). San Antonio, TX: International ATMO, Inc.
- National Fire Protection Agency (NFPA). (2021). “NFPA 99 2021 Edition: Health Care Facilities Code.” Quincy, Massachusetts.
- Undersea and Hyperbaric Medical Society MEDFAQ: “Regarding the Hyperbaric Safety Director for a hospital based hyperbaric department,” Accessed 3/8/21 Link
- Workman, W. T., & Wood, J. S. (2020). Hyperbaric Facility Safety: A Practical Guide (2nd ed.). Best Publishing Company.
Respectfully,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I am asking this question because the 2018 FGI Guidelines for Design and Construction of Hospitals references the UHMS in Section A2.2-3.13.1.2 as a contact for additional information. I am an architect, and we are currently in the schematic design phase for a Wound Care Center that will house 3 Monoplace Chambers.
Posted: 10/14/2020
Your question was reviewed by the Hyperbaric Oxygen Safety Committee of the Undersea and Hyperbaric Medical Society (UHMS). Our committee can provide you with additional information to assist your decision-making, but please keep in mind that your local Authority Having Jurisdiction (AHJ) is ultimately responsible for interpreting the facilities’ classification. Neither the UHMS nor the HBO2 Safety Committee assume any responsibility in this regard as we are not a governing body. The HBO2 Safety Committee’s responses are listed below in red.
Good Morning,
Q: I am asking this question because the 2018 FGI Guidelines for Design and Construction of Hospitals references the UHMS in Section A2.2-3.13.1.2 as a contact for additional information.
I am an architect, and we are currently in the schematic design phase for a Wound Care Center that will house 3 Monoplace Chambers.
A: NFPA 101 invokes the occupancy requirement of Ambulatory Healthcare whenever 4 or more patients are rendered incapable by the procedure. Although ambulatory when they arrive at the facility, hyperbaric patients in the monoplace chamber are rendered incapable of taking actions for self-preservation for the duration of the time they are in the chamber. If there is potential that the facility could expand in the future to 4 or more chambers, the facility should consider building to Ambulatory Healthcare during the initial buildout. CMS Memo S&C-11-05-LSC has been interpreted by some AHJ’s as requiring Ambulatory Healthcare regardless of the number of monoplace chambers installed. This is the case in the state of Colorado and has led to general best practice recommendations that facilities consider Ambulatory Healthcare regardless of the number of chambers.
Although this strictly Outpatient facility will be located in a Medical Office Building (not a Hospital setting) with standard office hours of 8 a.m. – 6:00 p.m, it will be operating under the hospital umbrella as far as licensure goes. The point to that statement is, although Hyperbaric chambers are provided for, under the above noted FGI, there are no requirements under the FGI Guidelines for the Design and Construction of Outpatient Facilities.
When designing under the “Hospital” Guidelines, the below are required.
- A generator with at least 24 hours of fuel, unless it’s in an area which could have extended outages. In that case, the minimum would be 96 hours.
A: A generator is not required unless the hyperbaric facility will treat emergent hyperbaric indications and use ancillary medical devices. The monoplace chamber is run by gas pressure versus electrical power. An exception to this rule of thumb exists in the state of Colorado. In recent years Colorado has required hyperbaric facilities to have a backup generator or a suitably sized battery UPS to provide emergency power for pneumatically operated chambers. - A separate electrical room for transfer switches and emergency switchgear
- All panelboards would need to be in rooms rather than in corridors
- Increased receptacle counts in all patient care areas
A: The standard receptacle count for business occupancy should generally meet the needs for patient care areas. Outfitting of the patient care area with computers, monitors, podiatry chairs, procedure lamps, and etc. should be taken into consideration when determining outlet count and locations. - HVAC equipment would likely need to be on emergency power
A: See response to bullet #1. The internal temperature of the monoplace chamber is primarily regulated by ambient room temperature and chamber ventilation settings. Thus, if treating emergent indications, the HVAC should be tied to the emergency power, should there be a loss of power.
REFERENCES:
Centers for Medicare and Medicaid Services (CMS). (12/17/2010 REVISED 02/18/2011). “S & C-11-05-LSC: Hospital and Critical Access Hospital (CAH) Facility Life Safety Code (LSC) Occupancy Classification Update”. Baltimore, Maryland. DEPARTMENT OF HEALTH & HUMAN SERVICES (Accessed 10/13/2020)
National Fire Protection Agency (NFPA). (2018). “NFPA 99 2018 Edition: Health Care Facilities Code, “Chapter 14 – Hyperbaric Facilities”. Quincy, Massachusetts.
National Fire Protection Agency. (2018). NFPA 101: Life Safety Code, “ 3.3.190.1, 6.1.6, A6.1.6.1”. Quincy, Massachusetts.
Undersea and Hyperbaric Medical Society. (2018). Clinical Hyperbaric Facility Accreditation Manual (4th ed.), “HBOC 1.0 – HBOC 4.0: Facility Construction”. North Palm Beach, FL: Undersea and Hyperbaric Medical Society, Inc.
Thank you for reaching out to the UHMS and please contact us if you have any further questions.
Sincerely,
The UHMS HBO2 Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I visited a gym in Illinois that offered hyperbaric chamber services to their members. I would like to possibly add hyperbaric treatment options to my business as well. Where can I go to find out what I would need to do so in Minnesota?
Posted 8/25/2020
Q:
I visited a gym in Illinois that offered hyperbaric chamber services to their members. I would like to possibly add hyperbaric treatment options to my business as well. Where can I go to find out what I would need to do so in Minnesota?
A:
Thank you for your inquiry regarding your interest in hyperbaric oxygen therapy. My name is Andrew Melnyczenko, chair of the UHMS Safety Committee, and your question was recently forwarded to me by the executive director of the UHMS.
Members of the UHMS Hyperbaric Oxygen Safety Committee are in agreement with existing position statements formed by trusted professional hyperbaric entities against the practice of providing hyperbaric oxygen therapy outside of a clinical or hospital-based setting. It is important to recognize that hyperbaric facilities must comply with mandatory federal, state and local codes governing the design, construction, installation and operation of hyperbaric chambers. These continuously evolving safety standards are established to protect patients, staff, and medical facilities. It should be noted that any facility that has been accredited by the Undersea and Hyperbaric Medical Society must meet these requirements.
Furthermore, the provision of hyperbaric treatment without the administration of oxygen has shown no beneficial health effects. Medical grade oxygen meeting the purity standards for human use as defined by the United States Pharmacopoeia (USP) must be prescribed by a licensed medical practitioner, and in this case one with specific training in the combination of oxygen used under hyperbaric conditions.
I encourage you to review the following position statements from the UHMS, the National Board for Diving and Hyperbaric Medical Technology (NBDHMT), Health Canada, the Food and Drug Administration (FDA) and other pertinent articles referenced below. You will also find references describing the dangers of soft-sided chambers, but please be aware that all hyperbaric chambers are engineered medical devices that may incur serious risk to everyone involved regardless of the type of chamber used.
I am obliged to provide you with these educational resources as a warning, and I implore you to reconsider any plans to offer hyperbaric therapy outside of a UHMS-accredited hospital or clinic-based facility. If you have any additional questions, I would be happy to discuss this further. Thank you once again for reaching out to the UHMS – this indicates to me that you are seeking to understand the dangers associated with non-compliance and the serious risks associated with hyperbaric oxygen therapy.
- UHMS Position Statement
- NBDHMT Position Statement - Portable, Fabric, Low-pressure Hyperbaric Chambers
- NBDHMT Position Statement - In-Home HBO
- The Food and Drug Administration (FDA) – “Hyperbaric Oxygen Therapy: Don't Be Misled”
- National Fire Protection Association (NFPA) Journal - "The Air in There"
- Health Canada: "Unauthorized soft-shelled hyperbaric chambers may pose serious health risks"
Sincerely,
Andrew R. Melnyczenko
Safety Committee Chair
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I’m looking for care for my mom. I’d like to find a doctor that can come to our house. I purchased a hyperbaric chamber for treatments. My mom suffered from a stroke a year ago and I’d like to get some treatments for her to speed up her recovery.
Date: 8/25/2020
From: UHMS HBO2 Safety Committee
Q:
I’m looking for care for my mom. I’d like to find a doctor that can come to our house. I purchased a hyperbaric chamber for treatments. My mom suffered from a stroke a year ago and I’d like to get some treatments for her to speed up her recovery.
A:
Thank you for your question. The UHMS HBO2 Safety Committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions would normally reside with a medical director and safety director of a hospital or clinic-based hyperbaric facility.
References:
- UHMS Position Statement
- NBDHMT Position Statement - Portable, Fabric, Low-pressure Hyperbaric Chambers
- NBDHMT Position Statement - In-Home HBO
- The Food and Drug Administration (FDA) – “Hyperbaric Oxygen Therapy: Don't Be Misled”
- National Fire Protection Association (NFPA) Journal - "The Air in There"
- Health Canada: "Unauthorized soft-shelled hyperbaric chambers may pose serious health risks"
- Locator - UHMS Accredited Clinical Hyperbaric Facilities
DISCLAIMER
I have a question for you. I thought I had the answer to this from when I worked in a mono place setting but the question has come up again. As long as there is a CHT present in the clinic, can a non CHT operate a multi place panel for a treatment?
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Regarding: A chamber operator qualifications.
Thank you for your question. There a several answers to this question and the comments below would apply to both class A and class B chambers. The responsibility of staffing complement falls to the Medical Director and the Safety Director, depending on staff qualifications / experience, type(s) and number of chambers, number and acuity of patients, location of the chamber(s) (hospital or freestanding clinic?) and number of patients treatments occurring simultaneously.
NFPA 99 Health Care Facilities Code, 2018 edition, 14.3.1.4.6 requires that during chamber operations , with occupant(s) in the chamber, the operator be physically present and maintain visible and audible contact with the control panel and chamber occupants. It is important that a qualified chamber operator be present during chamber operations. Please reference the Annex note under A 14.3.1.3.2.
The definition of “Qualified Person” is important to this topic. For this reply, the definition is taken from the NFPA 99, 2018 edition, 3.3.151, “Qualified Person. A person who, by possession of a recognized degree, certificate, professional standing, or skill, and who by knowledge, training, and experience, has demonstrated the ability to do the work.”
There are other standards and regulations in place outside of the USA. In the USA, we are aware of at least one state, (Ohio) that requires the chamber operator to be a CHT.
If you are preparing for a UHMS Hyperbaric Facility Accreditation survey, there are line items you will need to address. These include, accreditation concentration areas, Hyperbaric Operations, HBOO1.4 “During manned operations, the hyperbaric chamber operator is physically present and maintains visual or audible contact with hyperbaric chamber control console at all times.”, and Hyperbaric Human Resources, HBOHR 2.2 “At least one Clinical Hyperbaric Registered Nurse (CHRN) or Certified Hyperbaric Technologist (CHT) is on duty in the clinical area at all times when a patient is receiving hyperbaric treatment”, HBOHR 2.3 “A minimum of one hyperbaric technician or trained hyperbaric staff member is on duty in the hyperbaric facility when non-treatment hyperbaric chamber operations are ongoing.”
The UHMS Guidelines for Hyperbaric Facility Operations, 2nd edition also lists requirements for staffing class A and class B hyperbaric chambers.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
We have 2 monoplace chambers and are looking to upgrade our treatment area. What type of flooring is acceptable?
The UHMS safety committee is not in a position to make recommendations on flooring material in a hyperbaric chamber room. We can provide some guidance that may help you in your decision process.
- We suggest you contact your chamber manufacturer and review their recommendations or requirements for additional guidance.
- The National Fire Protection Association (NFPA) 99 Health Care Facilities, 2018 edition, chapter 14 Hyperbaric Facilities, does not specify the type of material for the flooring of a monoplace room, only that the floor be able to carry the weight.
- NFPA 101, Life Safety Code 2018 edition requires that all hyperbaric facilities regardless of the occupancy be treated as a health care facility. NFPA 101 Interior floor finish shall comply with 101, 10.2. You will need to make certain that the tiles you choose meet 101 and your local authority having jurisdiction (AHJ) approval.
- We are aware of facilities that use conductive tiles or conductive wax finish.
- We are aware of facilities that have chosen to use nonconductive tiles and apply a standard wax to protect the flooring.
- We are aware of several facilities that use VCT or seamless sheet vinyl flooring.
- The user should verify that the selected flooring has an indentation rating capable of handling the weight of the chamber and the patient.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is equipment with a brush motor prohibited in a mutiplace environment? When searching the NFPA 99, 2018 version I could not find anything specific about a brush motor in the hyperbaric environment.
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information, guidance and an opinion; however, the ultimate responsibility for these types of questions lies with the medical director and safety director of your facility.
SC Reply: Regarding brushed motors in the multiplace environment.
Brushless DC motors do not spark as they do not have brushes (satisfies the intention of NFPA 99, 2018, 14.2.9.3.11 & 14.2.9.3.13). For this reason, they are considered to be safer, especially where contained in a pressure-proof housing, or purged so as not to allow oxygen-enriched air to enter. These are user-specific decisions, based on risk assessment & mitigation. In short, we see brushless DC motors in purged housings being used.
The SC is not aware of specific wording in regulation to this effect as it could lead to misunderstandings as to what is safe. It is only safe if the risk is identified & understood, and mitigated.
The requirement for motors is stated in NFPA 99 as follows:
14.2.9.3.13 Exposed Live Electrical Parts.
No exposed live electrical parts shall be permitted, except as specified in 14.2.9.3.13.1 and 14.2.9.3.13.2.
14.2.9.3.13.1 Exposed live electrical parts that are intrinsically safe shall be permitted.
14.2.9.3.13.2 Exposed live electrical parts that constitute patient monitoring leads, which are part of electromedical equipment, shall be permitted, provided that they
meet the requirements of 14.2.9.3.17.
14.2.9.3.14* Motors.
Motors located in the chamber and that are not a component of medical equipment shall meet one of the following requirements:
(1) They shall comply with 501.125(A)(1) of NFPA 70.
(2) They shall be totally enclosed in accordance with 501.125(A)(2) or 501.125(A)(3) of NFPA 70.
and
14.2.9.3.17 Portable Patient Care–Related Electrical Appliances.
14.2.9.3.17.1 The appliance shall be designed, constructed, inspected, and maintained in accordance with Chapter 10.
Referring to the NEC (NFPA 70), 2014 (draft version):
501.125 Motors and Generators.
(A) Class I, Division 1. In Class I, Division 1 locations, motors, generators, and other rotating electrical machinery shall be one of the following:
(1) Identified for Class I, Division 1 locations
(2) Of the totally enclosed type supplied with positive pressure ventilation from a source of clean air with discharge to a safe area, so arranged to prevent energizing of the machine until ventilation has been established and the enclosure has been purged with at least 10 volumes of air, and also arranged to automatically de-energize the equipment when the air supply fails
(3) Of the totally enclosed inert gas-filled type supplied with a suitable reliable source of inert gas for pressurizing the enclosure, with devices provided to ensure a positive pressure in the enclosure and arranged to automatically de-energize the equipment when the gas supply fails.
One can also refer to the NFPA 99, 2018 section on switches (which is what the brushes in a DC electric motor do):
14.2.9.3.11 Switches.
Switches in the fixed wiring installation shall be waterproof.
14.2.9.3.11.1* Switch make and break contacts shall be housed in the electrical enclosure so that no sparks from arcing contacts can reach the chamber environment.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnoses or recommendations for equipment over the internet. The responsibility for medical diagnoses and treatments resides with the medical director; approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only.
Is there any regulation covering safety issues associated with interrupting or distracting the HBO2 Tech during an initial treatment, thus placing the patient at risk d/t the potential break in observation? As clinical coordinator I have argued that during treatments, the HBO2 room (we have one monoplace chamber) be regarded as off limits for ordinary business that can wait, and in the instance of initial treatments, off limits to all but the supervising HBO2 physician.
SC Regulations covering safety issues concerned with distracting the chamber operator.
The SC is not aware of a specific regulation regarding the disruption of the chamber operator during an initial treatment.
NFPA 99, 2018 chapter 14, has several requirements that are related to this question:
14.3.1.1.4.6 Requires that the chamber operator must be physically present and maintain visible and audible contact with the patient and / or chamber console during manned operations.
14.2.1.1.7 Requires that when used for hyperbaric operations the room or rooms housing the chambers shall be for the exclusive use of the hyperbaric operation.
The intent is to insure that the chamber operator is present and that there are only HBO2 related activities going on in the room housing the chamber during manned operations.
The UHMS facility Accreditation surveyors will also look for the chamber operator present during manned operations as per NFPA 99.
The FAA does have a requirement for pilots, that points to the concern of distractions during critical procedures:
Distracted driving is a major concern for all of us on the roads.
The initial treatment for a patient can be a critical event, where any difficulty pressurizing or anxiety with the new experience may impact their willingness to continue therapy. These things including other emergencies, can occur at any time, and not just the initial treatment. We recognize the concern with distracted chamber operator being a potential safety hazard. This is a risk that is managed on the local level. We also recognize that there can be HBO2 related activities occurring in the chamber area. We encourage you to work with your medical director, administration and the hyperbaric safety director to create a procedure that answers your concerns in your specific conditions.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members can provide medical diagnoses or recommendations for equipment over the internet. The responsibility for medical diagnoses and treatments resides with the medical director; approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only.
Our hyperbaric unit is a HOPD, are we required to have a carbon monoxide (CO) detector?
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Regarding: CO Monitor required in the hyperbaric suite.
The CMS has adopted the 2012 Edition of NFPA 101, Life Safety Code and NFPA 99, Health Care Facilities Code, therefore the Joint Commission and others are also referencing those documents during surveys. We do not know the occupancy classification of your building, it may well be that a carbon monoxide monitor is required.
The 2012 edition of NFPA 101 9.8 Carbon Monoxide (CO) Detection and Warning Equipment states that; “Where required by another section of this Code, carbon monoxide (CO) detection and warning equipment shall be provided in accordance with NFPA 720, Standard for the Installation of Carbon Monoxide (CO) Detection and warning Equipment”
We would encourage you to work with your safety personnel, industrial hygienist and follow the guidance of the surveyor. CO monitors are not expensive and are valuable tools for the safety of your staff and patients.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is it allowable to use a "clean agent" extingishing system in place of sprinklers in a center with monoplave chambers. I cannot find anything in the NFPA99 book regarding clean agent systems.
Published Date: 05/2017
Updated: 01/06/2026
Q:
Is it allowable to use a "clean agent" extinguishing system in place of sprinklers in a center with monoplace chambers. I cannot find anything in the NFPA99 book regarding clean agent systems.
A:
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
Current code language would allow a Clean Agent extinguishing system.
NPFA 99, (2024) Health Care Facilities, states:
A.14.2.1.2(3) When selecting a clean agent fire protection system, careful consideration should be given to the selection of agent based on permissible exposure levels.
The Vinegar, et al. PBPK data for HFC-227ea (FM-200) is shown in Figures 6-8A and 6-8B.
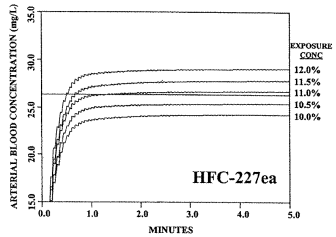 |
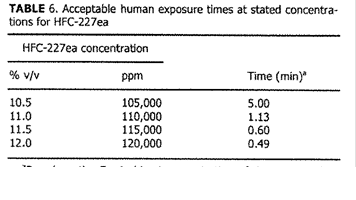 |
| Figure 6-8A. Graphical PBPK Data for FM-200 | Figure 6-8B. Tabular PBPK Data for FM-200 |
References:
National Fire Protection Agency (NFPA). (2024). NFPA 99 2024 Edition: Health Care Facilities Code. Quincy, Massachusetts.
NFPA 2001: Standard on Clean Agent Fire Extinguishing Systems, 2018 Edition, NFPA, Quincy, MA
Vinegar, A., Jepson, G. W. “Physiologically Based Modeling of Halon Replacements for Human Safety Evaluation.” Toxicological Assessment of Human Health Consequences Associated With Inhalation of Halon Replacement Chemicals, Next-Generation Fire Suppression Technology Program (NGP). Final Report. Project 3B/1/89. Section 1 of 2., ManTech Environmental Technology, Inc., Dayton, OH April 3, 2000.
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Figure 6-8A. Graphical PBPK Data for FM-200
Is there any regulations concerning the entry door(s) to a chamber room being secured with a punch code system?
I work in a clinic setting with wound care on one side of the building and I am alone on my side with HBO2. My boss would like to put a push button code lock on my door and I'm wondering if this is permitted? If there was a fire I'm concerned about the Fire Department not being able to get in. Does anyone have a similar issue? Is it ok to have this type of device on the HBO2 room door? We need some type of Safety policy and procedure for an active gunman in the building and I’m not sure how to go about this.
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Security is a real concern and we agree that Hyperbaric Facilities need to develop Policy and Procedures to manage active shooter / Code Silver, Bomb threats and other security concerns. We are required by NFPA 99, chapter 14, to have emergency drills on a regular basis. These threats should be added to your emergency response plans.
The SC would refer you to your local Authority Having Jurisdiction (AHJ). There are codes and regulations regarding locked doors. For guidance you can start with NFPA 101 Life Safety Code, 2012 edition, 7.2.1.5 Locks, Latches and Alarm Devices and NFPA 99, 2012 edition, Chapter 13, Security Management. Work with your local AHJ and Safety and Security department, possibly Emergency Management, to complete a threat assessment. These resources will help decide if a key pad is necessary.
In general we see no issue with a cipher lock on the entrance to the hyperbaric suite. In fact, we are aware of many facilities with ID badge, card access, push button locks and even keyed doors entering the room housing the chamber(s). The Fire Department will be able to gain access in the event of an emergency. Consideration should be given to enabling not only the Fire Department, but other responders such as code teams or security. The chamber room can be considered a restricted area, with authorized entry only. The concern is that evacuation in the event of an emergency is not hindered. There must always be an exit path, and the lock mechanism must not impede egress (or ingress of authorized personnel).
We also note that a chamber operator working alone is concerning. NFPA 99, 2015 edition, chapter 14 requires that there be a qualified chamber operator at the control panel with visual and audible communication with the occupants any time the chamber is in use. We would encourage the use of the UHMS Guidelines for Hyperbaric Facility Operations, 2nd edition, Section 3, Staffing Guidelines, to staff the chamber operation. Consider how to insure the safety and security of the single operator and any patients being treated, as described in this question. Is there a communications link for immediate help? Consider a panic button or regular rounding (closed circuit video feed?) by someone to check on the chamber operator and patients to provide support as needed. During your emergency drills, do you have the help you need to manage the number of patients?
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
What is the evidence for limiting linens in a monoplace chamber to a minimum of 50% cotton/polyester blend? I understand the fire risks of synthetic fibers, but why is the cutoff 50%?
Published Date: 11/2016
Review Date: 11/2019
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
The SC recommends submission of the question to the National Fire Protection Association, NFPA, 99 Health Care Facilities Code (http://www.nfpa.org). The NFPA has a process for the formal interpretation of these types of questions. There are several members of the SC that are also committee members of NFPA 99. Therefore, we need to add the disclaimer that this is our opinion and not a formal interpretation of the NFPA code. Please see an excerpt below copied from the 2018 NFPA 99, Health Care Facilities Handbook:
14.3.1.6.4.1 Except where permitted in 14.3.1.6.4.3, silk, wool, or synthetic textile materials, or any combination thereof, shall be prohibited in Class A or Class B chambers.
14.3.1.6.4.2 Garments permitted inside of chambers shall be as follows:
(1) Garments fabricated of 100 percent cotton or a blend of cotton and polyester fabric shall be permitted in Class A chambers.
(2) Garments fabricated of 100 percent cotton, or a blend of cotton and polyester fabric containing no more than 50 percent polyester, shall be permitted in Class B chambers.
Why is this important?
The intent of this paragraph is to make common textiles an option in hyperbaric chambers. The amount of polyester is limited in Class B chambers to reduce the amount of static electricity. In general, cotton generates less static charge than synthetic material. However, pure cotton tends to produce lint, and accumulated lint or dust in a hyperbaric chamber is an easily ignitable fuel. Selection of textiles for the hyperbaric chamber should be based on a variety of factors, including comfort, lint production, ignition temperature, static-producing properties, and fuel load of the material. The percentage of polyester in a cotton/polyester blend can have an effect on all of these factors.
Since the 2015 edition of the NFPA 99 code, a differentiation was made between the garments permitted inside of Class A and those permitted in Class B chambers. There is a maximum limit on the percentage of polyester permitted in blends that are allowed in Class B chambers. This is based on the different risks for each type of chamber. Class A chambers typically maintain an oxygen concentration below 23.5 percent and have fire suppression capability; the opposite can be said for Class B chambers.
A.14.3.1.6.4.2 Selection of textiles for the hyperbaric chamber should be based on a variety of factors, including comfort, lint production, ignition temperature, static-producing properties, and fuel load of the material. The amount of polyester in a cotton/polyester blend will likely have an effect on all of the factors.
Historically, all synthetic fabrics were prohibited from the chamber. Previous editions of this code allowed an “antistatic blend of cotton and polyester” because of one specific fabric – a blend of cotton and polyester with steel fibers to make it conductive. This blended fabric was intended for surgical scrubs, but its conductive properties made it a good choice for hyperbaric garments. The polyester in the fabric was acceptable because the conductive properties of the fabric actually afforded some protection from static production that cotton fabric did not. This particular fabric is no longer made. Selection of textiles has always been about balancing various safety concerns; primarily fire-resistance and static production. For further guidance on selecting appropriate textiles, see A.14.3.6.4.3.
14.3.5.6 All other fabrics used in the chamber, such as sheets, pillow cases, and blankets, shall conform to 14.3.1.6.4.1 and 14.3.1.6.4.2”
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
NFPA99 14.2.9.1.1 states all communication equipment inside a hyperbaric chamber shall meet the requirements set forth in 14.2.8.3.16 This states that the electrical "rating" of chamber speakers shall not exceed 28V rms and 25W. are we to assume that a higher rated speaker can be used inside the class B chamber? Just looking for little more clarification on this statement.
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Regarding: NFPA 99 14.2.9.1.1
The UHMS SC is not able to provide a formal interpretation of NFPA code. Jonathan Hart NFPA Staff Liaison, gave an informal response to this question in the NFPA XChange, members only section of the NFPA website. Mr. Hart has given us permission to duplicate his reply and disclaimer (below). In addition to Mr. Hart’s reply, the UHMS SC response can be found below.
Response from Jonathan Hart (NFPA):
“The answer from the language in the code is clear that there is no leeway provided. It applies to the maximum rating of the speaker and therefore any speaker with a rating higher would not be in compliance. An alternative approach could be argued under the Equivalency clause of Chapter 1 provided it were acceptable to the AHJ involved in the decision. My discussions with committee members on this topic indicate that there needs to be a bigger discussion within the committee next code cycle to determine the purpose of this clause and clarify if it is truly the rating we are worried about or the output of a system to the speaker itself. Because it is not clear as of now, the code has to stand on its own as written.
Important Notice: Any opinion expressed in this correspondence is the personal opinion of the author and does not necessarily represent the official position of the NFPA or its Technical Committees. In addition, this correspondence is neither intended, nor should it be relied upon, to provide professional consultation or services.”
Response from UHMS SC:
Throughout the Hyperbaric Facilities chapter of NFPA 99 (2015 edition), one consistent protection strategy is to limit power levels in Class B (monoplace) chambers more so than in Class A chambers. To this end, communication systems for Class A and Class B chambers are addressed differently in different sections of the code. Section 14.2.8.3* Wiring and Equipment Inside Class A chambers, and all the subsections of 14.2.8.3 were intended for multiplace chambers. Section 14.2.8.6 Additional Wiring and Equipment Requirements inside Class B chambers, was intended for monoplace chambers.
The wording of paragraph 14.2.9.1.1 implies that all communications equipment located inside a chamber (monoplace or multiplace) should comply with the requirements of the section intended for multiplace chambers. Because of the difference in power limits, it would be inappropriate for monoplace chambers to use electrical design rules from a section intended for multiplace chambers. A Tentative Interim Amendment (TIA) to NFPA 99 has been proposed to alter the wording of paragraph 14.2.9.1.1 in order to avoid future confusion about this issue.
We would encourage you to get involved with the NFPA code process. The 2018 edition of NFPA 99 is in its second draft and there is no mechanism to add new business at this point. If you have specific changes you would like to see, please consider making a public input for the 2021 edition of NFPA 99 when that cycle is open.
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
I am unable to find documentation regarding specifications for the required smoke hood for multiplace chambers. The ones we have on hand are about to reach their expiration date & that particular brand does not seem to be available at this time. There is
Published Date: 5/2016
Review Date: 5/2019
Due Review: 5/2022
The National Fire Protection Association, NFPA 99 Health Care Facilities Code, 2018 edition, chapter 14: 14.2.4.5.3* states, “A means for respiratory and eye protection from combustion products allowing unrestricted mobility shall be available outside a Class A or Class B chamber for use by personnel in the event the air in the vicinity of the chamber is fouled by smoke or other combustion products.”
This requirement may be met by several different devices; these range from umbilical-supplied smoke hoods and self-contained breathing apparatus, to the emergency escape hoods. Whichever device you choose, you must also meet any OSHA and local authority requirements for training, maintenance, documentation and medical fitness to wear the device.
NFPA does not specify the type of device only that you have one.
We suggest that the selection of the device depends on the type of chamber and patients treated at your facility, together with the degree of emergency support to the unit, the distance to the nearest area of safety and the number of patients that need to be evacuated. These factors have a bearing on the length of time that the operator needs to be able to remain in a smoke-filled area. Emergency drills with the various devices should be carried out to evaluate how they will work in your environment. Work with the manufacturer of your facility and engage the industrial hygienist in your hospital. Document your decision process, maintenance and training. The
UHMS accreditation survey probes HBOV 2.0, 2.1, 2.2, 2.3, 2.4 and 2.5 addresses this question as well. The survey does not specify the type of alternative breathing air apparatus.
For references see:
- NFPA Mandated SCBA Type Capability Within Clinical Hyperbaric Facility: An Analysis of the Types and Frequency of use, Canterbury B; Baker B
- Chamber Fire Safety, Schmidt, TC; Dorr VA; Hamilton JR RW
- Selecting Smoke Hoods for Hyperbaric Facilities, Wood S
- NFPA 99, 2015 edition, chapter 14 Hyperbaric Facilities
- UHMS Clinical Hyperbaric Facility Accreditation Manual (Rev1)
- NIOSH, “NIOSH RESPIRATOR SELECTION LOGIC,”
- OSHA Regulations standard 29 CFR personal protective equipment 1910.134 respiratory protection
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Regarding the Hyperbaric Safety Director for a hospital based hyperbaric department (monoplace chambers)
Published Date: 5/2016
Review Date: 5/2019
Due Review: 5/2022
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Question; Regarding the Hyperbaric Safety Director for a hospital based hyperbaric department (monoplace chambers):
- Does NFPA 99 require the Hyperbaric Safety Director to be on premise when chambers are operating?
- Is it ok for them to be available by phone?
- If someone is covering for the Hyperbaric Safety Director when they’re unavailable, i.e. on vacation:
- Does the covering person need to have Hyperbaric Safety Director Training?
- Would the Hospital Safety Director (not involved in daily hyperbaric operations) be an approved choice?
Regarding: Hyperbaric Safety Director (HSD) requirement to be on premises when chambers are operating.
It is the responsibility of the administration, medical director and safety director to compile a policy and procedures for the type of chambers, acuity of patients and qualifications of staff.
- Language requiring an individual with the responsibilities of hyperbaric safety director (HSD) has been in NFPA 99 since 1970 (56D). NFPA 99, 14.3.1.3.2 requires that each facility designate an on-site hyperbaric safety director (HSD). We are not aware of any requirement in NFPA 99 that specifies that the hyperbaric safety director be on the premises when chambers are in operation.
There is further information on this topic in the annex of NFPA 99 A14.3.1.3.2. The complexity of hyperbaric medicine is such that one person should be designated as the chamber operator. That person should be knowledgeable and have the training and experience to recognize hazards.
NFPA 99, 14.3.1.4.8 requires that a chamber operator be physically present and maintain visual and audible contact with the control panel or chamber occupant(s) during hyperbaric oxygen therapy.
The UHMS facility accreditation probe HBOHR 2.2 looks for a Certified Hyperbaric Nurse or CHT on premises when chamber operations are going on. - It is acceptable for the HSD to be available by phone, and in our experience, this position is most often available 24/7 for calls regarding the hyperbaric facility.
- If the HSD is not available, on vacation or other, there needs to be an alternate HSD named to be responsible. It is good practice to bring staffing “up” in the department and have a succession plan in place.
- The individual covering for the HSD should have attended a hyperbaric safety director course, have knowledge and experience in hyperbaric medicine and with the equipment used at the facility. This could be the lead chamber operator with the most experience, for example.
- Unless the hospital safety director has knowledge and experience with hyperbaric medicine and has attended a hyperbaric safety director course, we would not encourage using this resource to cover the HSD absence. We would encourage working closely with the hospital safety director so that individual has some knowledge of our unique practice.
For references see:
MEDFAQ July 07, 2015 regarding safety director training
NFPA 99, 2018 edition, chapter 14 Hyperbaric Facilities
UHMS Guidelines for Hyperbaric Facility Operations, 2nd edition
UHMS Clinical Hyperbaric Facility Accreditation Manual (Rev1)
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Are there current guidelines pertaining to the number of HBO2 technicians that need to be present during a hyperbaric treatment?
Published Date: 5/2016
Review Date: 5/2019
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
The National Fire Protection Association (NFPA) 99 Health Care Facilities Code, 2018 edition 14.3.1.4.2 States that the medical director and safety director shall jointly develop the minimum staffing qualifications, experience, and complement based on the following.
- Number and type of hyperbaric chambers in use
- Maximum treatment capacity
- Type of hyperbaric therapy normally provided
The UHMS Guidelines for Hyperbaric Facility Operations, 2nd edition provides guidance in section 3, Staffing Guidelines.
The UHMS position statement: Minimum-staffing guidelines of multiplace hyperbaric facilities: Click here for paper
Posted September 2018 at https://www.uhms.org
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Are HBO centers required to have EKG/ECG monitoring equipment readily available?
Published Date: 5/2016
Review Date: 5/2019
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
This depends on the acuity of the patients you are treating and the qualifications of the medical staff: this should be congruous with your stated scope of services. We are not allowed to lower the level of care. For facilities in a Health Care that would mean, yes, you would need to be able to monitor EKG/ECG as there will most likely be inpatients or emergencies where monitoring would already be in place and to discontinue it would be incorrect.
For a facility with outpatients only, this might mean that you would not be required to monitor patients with EKG/ECG during hyperbaric oxygen therapy. We would caution you to be aware of the patient population you serve and especially the stated scope of such services.
If you do monitor this also implies that you have qualified personnel available that can interpret what they are seeing on the monitor and provide ACLS / BLS support as necessary. It also stands to reason that any equipment used to monitor patients must be integrated safely into the chamber system.
For reference please see:
NFPA 101, 2018 edition, Chapter 3 Definitions, 3.3.196.7* Health Care Occupancies, https://www.nfpa.org accessed 6-4-2019
UHM 2016, Vol.43, No1 – Hyperbaric programs across the United States. Walter Chin, Laura Jacoby, Olivia Simon, Nisha Talati, Gracelene Wegrzyn, Rachelle Jacoby, Jacob Proano, Susan E. Sprau, Gerald Markovitz, Rita Hsu, Ellie Joo
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Can chambers be used for off-label treatment if it is not listed on the chambers 510K approval?
Published Date: 03/2016
Review Date: 03/2019
Due Review: 03/2022
Thank you for your question. The UHMS HBO safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety director of your facility.
The Food and Drug Administration (FDA) does not practice medicine. The 510K premarket notification is a manufacturer’s document submitted to the FDA. A physician may use a device outside of the parameters listed on the 510K. This is a practice known as “Off-Label” use of a drug or device by a physician as their license allows. However, they cannot advertise or market the fact that they are using the drug or device for an off-label indication. The marketing restriction applies not only to the manufacturer but to the user of the device. The FDA has issued warning letters to facilities to promoting the use of a hyperbaric chamber for off-label indications. However, if a physician deems it in the best interest of the patient, he or she may use a device for something for which its approval was not given.
Physicians have a responsibility to justify any medical decision, utilizing good judgment and proper risk management. They must be able to provide this justification before their peers. For example; using a ventilator in a chamber which does not have FDA clearance is not improper, so long as it is a medical device and the physician has assessed all of the risks prior to use.
Considerations for using a “bag” chamber or any hyperbaric chamber for non-approved indications:
- If a physician does this, his controlling body should surely sanction this?
- If advertised as medicine, then surely there are consequences if there is no healthcare practitioner?
- If the chamber is in a public place, surely the local fire marshal or pressure vessel inspector has some jurisdiction?
- In the USA the National Fire Protection Association (NFPA) 101 Life Safety Code refers any occupancy to the NFPA 99 Health Care Facility Code for hyperbaric medicine.
- The European College of Hyperbaric Medicine has stated: “If it is a non-recognized treatment, you can only do this as part of an ethically approved project and not for reimbursement.”
References:
The National Fire Protection Association, NFPA 101, Life Safety Code, 2018 edition
The National Fire Protection Association, NFPA 99, Health Care Facilities Code, 2018 edition
510(K) Definition: A 510(K) is a premarket submission made to FDA to demonstrate that the device to be marketed is at least as safe and effective, that is, substantially equivalent, to a legally marketed device (21 CFR §807.92(a)(3)) that is not subject to premarket approval. Source: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfpmn/pmn.cfm
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Is there a requirement for how much humidity is required in the room that houses monoplace chambers? I have looked at the NFPA and it addresses multiplace chambers.
Posted 2015
Update posted: 4/1/2025
Thank you for your question. The UHMS HBO2 safety committee can provide information to assist you in answering your question, but the ultimate responsibility for these types of questions rests with the medical director and safety coordinator of your facility.
There are no codes we are aware of specifically regarding humidity control in the monoplacehyperbaric suite.
It is accepted that greater than 60 percent humidity will nearly eliminate static potential. (A14.3.1.6.4.3*) Personnel states that antistatic procedures are under the safety coordinator’sresponsibilities whenever atmospheres greater than 23.5 % O2 are used. In our opinion this relates to the class A chamber not the room housing the chamber. A14.3.1.6.4.3 (3) discusses static and humidity in regards to a risk assessment for a wound dressing.
Grounding is a critical part of operating monoplace hyperbaric chambers. Ensure that the chamber and patient are grounded and document the findings.
Humidity is mentioned in an out-of-print UHMS guideline (pdf on the UHMS web site under Safety) and in the 2005 edition of the 101 Handbook for anesthetizing locations. Some monoplace facilities have added humidity controls to their rooms; some facilities have humidity as a function of the as built design of the HVAC system. The majority of monoplace hyperbaric suites we are aware of do not do anything in regard to controlling humidity in the room.
Some hyperbaric chamber manufacturer (OEM) manuals also call for a humidity range for safe chamber operation.
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
Can you provide a resource that outlines the inspection requirements for a monoplace chamber that has met the 10 year/10000 dive design life necessary for ongoing use of the chamber?
Thank you for your question. The UHMS hyperbaric oxygen safety committee (SC) can provide information but the ultimate responsibility for these types of questions is with the medical director and safety director of your facility.
Regarding the current ASME PVHO rules for a monoplace chamber that has met the 10 year / 10,000 cycle design life:
We advise you to purchase the most recent edition of ASME PVHO-2. If your department has a firewall we might suggest purchasing the hard copy instead of the pdf as the pdf is actually a link to the “cloud” and you may have trouble with using it with your hospitals IT security.
https://www.asme.org/products/codes-standards/pvho2-2016-safety-standard-pressure-vessels-human
As you know, the design life is 10 years. During that time, following PVHO-2 is optional.
There is a required 10-year Maintenance Viewport Inspection that in the past we had to pull the end plates off the monoplace in order to inspect the seals and portions of the acrylic that cannot be seen under the seal. This normally meant sending the monoplace chambers back to the manufacturer or having a third party come out and do this on site. The current edition of the code has an alternative method that can be used without dissembling the chamber.
The service life can be longer than the design life if you follow the rules of PVHO-2.
For medical systems in a protected environment that means adding 10 years, but you need to follow the rules for Operational, Maintenance and Seat & Seal inspections years 11-20. By default, the service life of monoplace chambers is currently 20 years. A multiplace has more windows and there are destructive testing rules for those windows.
The annual or 18-month Maintenance inspections need to be completed by a qualified person.
If you have not done so already we would strongly encourage you to send someone to an acrylic maintenance course. The owner of the vessel is responsible for training, record keeping and maintenance.
Respectfully,
The UHMS Safety Committee
DISCLAIMER
Neither the Undersea and Hyperbaric Medical Society (UHMS) staff nor its members are able to provide medical diagnosis or recommend equipment over the internet. If you have medical concerns about hyperbaric medicine you need to be evaluated by a doctor licensed to practice medicine in your locale, which can provide you professional recommendations for hyperbaric medicine based upon your condition. The responsibility of approving the use of equipment resides with the physician and safety director of the facility. Information provided on this forum is for general educational purposes only. It is not intended to replace the advice of your own health care practitioner and you should not rely upon it as though it were specific medical advice given to you personally.
