As we prepare to close the books on another year and usher in a new one, focus on our mission remains the priority.
We are facing significant challenges shaping our specialty. Challenges like the erosion of the practice of medicine, the decline in 24/7 urgent and emergent programs, the dismissive nature of some healthcare executives of the value clinical hyperbaric medicine brings to their patients and communities, and the yo-yo-ing of CMS policy and payment are top of mind.
Of those challenges, the latter one has us on edge. The UHMS QUAR Committee posted a message last week about an unexpected cut in the HOPD G0277 rate.
“The UHMS has become aware of a payment change published in the OPPS (Outpatient Prospective Payment) Final Rule for 2024. G0277, predicted to be about $134/30 minutes, was valued at $73.64 (national unadjusted reimbursement rate). There is a comment period for errors in the published document. Because there was no mention of hyperbaric oxygen in the Proposed Rule in July, there should not have been any substantive change in the Final Rule."
We believe this precipitous drop is a mistake on CMS’s part. However, our response options are limited because this rate is published in the Final Rule. So, the immediate goals are to get CMS’s attention about the significant reduction and, following, present data showing why the 2024 rate is an error.
We will achieve these goals by working alongside our Corporate Partners and the Alliance of Wound Care Stakeholders.
The other challenges I mentioned deserve the same intense attention from the field’s stakeholders as we’re devoting to the current payment issue. If we can do this, we will move the needle and control our destiny rather than be subjected to someone else’s.
On a far happier note, UHMS continues to expand its relationship with the Aerospace Medical Association (AsMA). After a successful joint meeting in Reno in 2022 and thoughtful consideration after reviewing the attendees’ feedback, both Governance teams agreed to hold joint Annual Scientific Meetings beginning in Atlanta in 2025 through 2030 in Houston, TX, when AsMA will celebrate its 100th anniversary.
This strategic alliance will benefit UHMS attendees in three ways. One, meeting costs, including hotel, will be lower as all rooms are negotiated at Government per diem rates; two, UHMS attendees will benefit from meeting locations we’ve typically been priced out of; and last, access to expanded relevant educational content.
This change will make our meeting next year in New Orleans much more memorable, especially with the smaller, more intimate venue at the Astor Crowne. Please join us and register early to reserve your room.
As I mentioned in my last note, next year’s election cycle has numerous officer and director positions coming open, including the President-Elect, Vice President, Treasurer, 2 Members-at-Large (MAL), including our MAL military active-duty, and Associate Nurse Representative-elect. Look for the call for nominations in mid-December.
UHMS Finances
Despite the challenges, UHMS continues to perform well financially; through October, UHMS’s financial position was positive.
|
Jan-Oct 2023 PL
|
| |
Actual
|
Budget
|
|
Income
|
1,313,312
|
1,248,565
|
|
Expense
|
1,260,946
|
1,259,648
|
|
Net
|
52,366
|
-11,083
|
Our balance sheet remains healthy, with operating, savings, and investment accounts continuing to hover at near-all-time highs.
Certification Matters
We continue to receive questions about technician and nursing certification. The UHMS’s position is unchanged in that we believe that all team members involved in providing care to patients in hyperbaric medicine should be certified, and our position statement - The Importance & Recognition of Hyperbaric Certification for Technicians & Nurses can be found here - UHMS POSITION STATEMENT.
Congratulations to the Q4 Associate Scholarship Award winners, Sarah Juba and Steph Simmons. They each are awarded tuition-free attendance to a UHMS-approved Introductory Course in Hyperbaric Medicine. Of course, this program is required to sit for UHMS-recognized hyperbaric certification exams.
Member Benefits
As a reminder, UHMS members receive three free CE/CME credits upon joining or renewing. This benefit represents an immediate $40 savings for Associate members and $60 for Regular members annually.
Associate Member Town Hall
Members are invited to attend the UHMS Associate Council town hall meeting on the second Thursday of every quarter, where invited speakers present on relevant topics that apply to our specialty.
Corporate Partners
If you are a UHMS Corporate Partner, please attend our monthly Corporate Partner Town Hall meeting series. These are held on the 1st Wednesday of every month at 12 PM and are intended to be an open forum for discussing the challenges and successes your businesses and practices are experiencing and to create momentum and collaboration where appropriate.
If your organization wants to educate the UHMS membership about the care provided or the goods and services offered, consider joining our Corporate Partnership Program. See https://www.uhms.org/corporate-memberships.html.
MEDFAQs
The UHMS offers its version of “ask the experts.” MEDFAQs can be found at the following URL – https://www.uhms.org/resources/medfaqs-frequently-asked-questions-faq.html, and is a valuable tool for our membership.
If you are familiar with MEDFAQs, check back, as new Q&As are posted regularly.
Research
The UHMS Research Committee continues to be very active. We hope to announce good news in the new year on the IRB front, where members of our community can come to the UHMS for their Institutional Review Board needs.
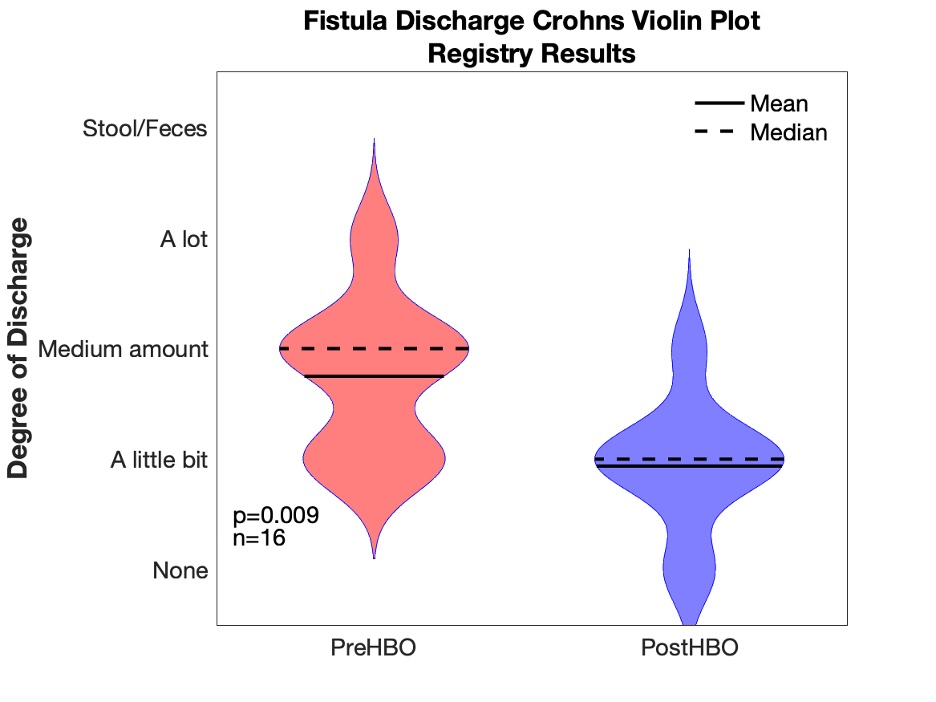
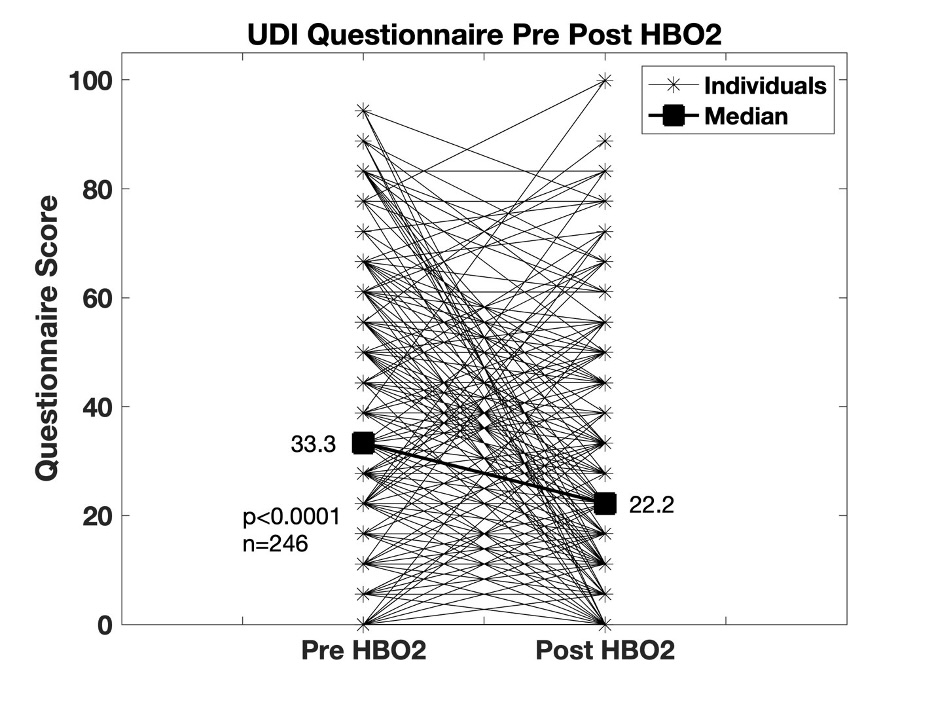
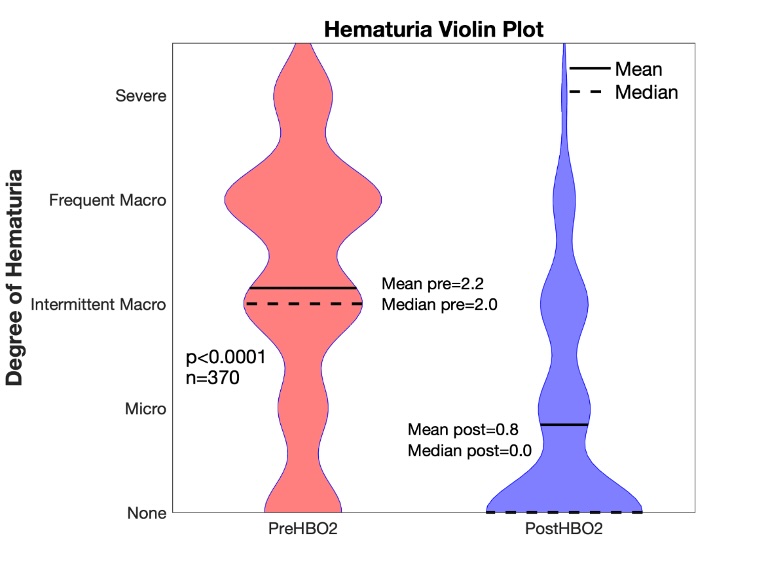
We are soliciting donations from our members for two research initiatives. One is the Continuous Glucose Monitor study (https://www.uhms.org/cgm-hyperbaric-oxygen-study), and the Multicenter Registry for Hyperbaric Oxygen Therapy at Dartmouth (MRHBO2) continues seeking funds for free hospital membership. The MRHBO2 is funded entirely via grants, not by the registry's participating hospitals - https://www.uhms.org/donate-to-the-multicenter-registry-for-hyperbaric-oxygen-therapy.html.
Remember that donations to the UHMS Funds for Research and Policy Advancement are tax-deductible. For more information, check out the UHMS website – https://www.uhms.org/funding.html.
QUARC
To better understand the field’s challenges, log in and visit the QUARC page – https://www.uhms.org/resources/quarc.html. Here, you will find impending legislation and other relevant policies on the provision and limitations of HBO2 coverage and the UHMS’s responses and guidance.
The chairs of QUARC are requesting that any unusual denials or challenges with physicians gaining access to insurance panels for HBO2 services, let us know as soon as possible, please – jpeters@uhms.org.
UHM
If you are a UHMS member, we are happy to announce a new search feature for previous issues and articles from UHM/UBR - https://www.uhms.org/publications/uhm-journal/download-uhm-journal-pdfs.html. Currently, the feature works with keywords.
If you have a suggestion or comment on how we can serve you better, please email me directly at jpeters@uhms.org or call me at 561-776-6110 extension 100.
It is my pleasure to serve you, our membership, and I continue to look forward to hearing from you.
John Peters

 _______________________________________________________
_______________________________________________________